- Esophageal motility disorders include disorders of hypomotility (e.g., achalasia) and hypermotility (e.g., diffuse esophageal spasm).
- Distal esophageal spasm (DES; corkscrew esophagus): premature and uncoordinated nonpropagative esophageal peristalsis in at least 20% of swallows
Epidemiology
Etiology
Pathophysiology
Clinical features
- Intermittent dysphagia to liquids (and potentially, solids)
- Dysphagia predominantly to solids is more suggestive of a mechanical obstruction, e.g., a esophageal stricture, cancer, or ring.
Diagnostics
Manometry
- Procedure: measures the amplitude, length, and duration of the peristaltic waves via a nasogastric tube fitted with numerous pressure sensors
- Findings
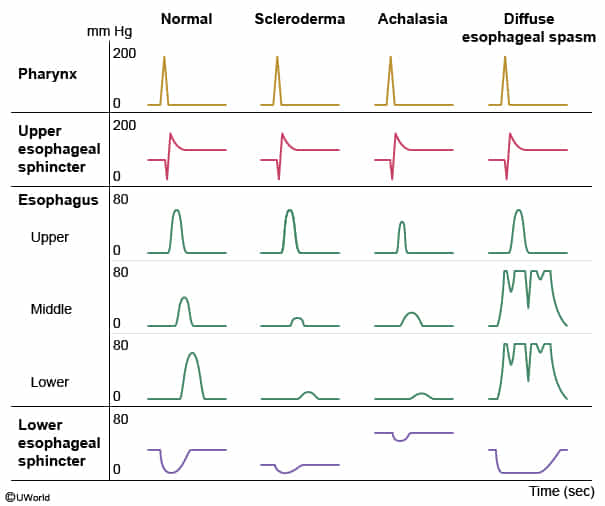
- Normal condition: To initiate swallowing, the contents of the oral cavity are collected on the tongue and propelled into the pharynx, where contraction of the pharyngeal muscles pushes the material into the esophagus. The cricopharyngeus muscle contracts behind the food bolus, initiating a peristaltic wave to propel the bolus downward. When the food bolus reaches the lower esophagus, the lower esophageal sphincter (LES) relaxes to allow the material to enter the stomach.
- Systemic sclerosis (scleroderma) can affect the esophagus, leading to impaired motility, incompetence of the LES, and gastroesophageal reflux disease. Manometry will show decreased peristalsis with decreased tone at the LES.
- Achalasia:
- A motility disorder caused by reduced numbers of inhibitory ganglion cells in the esophageal wall, which creates an imbalance favoring excitatory ganglion cells.
- This patient’s esophageal manometry shows typical findings in achalasia, including normal contraction of the upper esophageal sphincter, decreased amplitude of peristalsis in the mid esophagus, and increased tone and incomplete relaxation at the LES
- Diffuse esophageal spasm presents with severe, retrosternal chest pain. It is characterized by uncoordinated contractions of the esophageal body. Esophageal manometry shows intermittent peristalsis and multiple simultaneous contractions on tracings from the mid and lower esophagus.
- Esophageal stricture presents with progressive solid food dysphagia. It is diagnosed with contrast imaging (eg, barium swallow) rather than manometry. However, most patients will have a long history of gastroesophageal reflux with decreased tone at the LES.
- Distal esophageal spasm: premature contractions in at least 20% of swallows
- Disorganized non-peristaltic contractions on esophageal manometry and “corkscrew” esophagus on barium esophagogram
- Hypercontractile esophagus: hypertensive esophageal contractions in at least 20% of swallows
- HRM may be normal between acute episodes
Differential diagnostics
Esophageal motility disorders typically cause dysphagia with both solids and liquids. Dysphagia predominantly with solids is suggestive of a mechanical obstruction (intraluminal, mural, or extrinsic).
- Esophageal cancer (older age)
- Eosinophilic esophagitis (younger age)
- Esophageal webs or rings
- Esophageal diverticulum
- Extrinsic esophageal compression (e.g., hilar lymphadenopathy)