Etiology
- Risk factors for sporadic RCC
- Smoking
- Obesity
- Hereditary renal cell carcinomas
- Von Hippel-Lindau syndrome: Approx. 40% of patients with VHL syndrome develop renal cell carcinomas (usually clear cell RCC).
Pathology
- Renal cell carcinomas are adenocarcinomas that usually arise from the epithelial cells of the proximal convoluted tubule (80%).
- Because of high metabolic activity and exposure to toxins
- Clear cell renal cell carcinoma
- Frequency: 70%
- Etiology: Sporadic or inherited mutation of VHL gene on chromosome 3p
- Microscopic appearance:
- Polygonal cells arranged as cords or tubules (non-papillary growth)
- Clear, glycogen and/or lipid-filled cytoplasm
3: A mutation in the VHL (von Hippel-Lindau) gene on chromosome 3 causes RCC (renal cell carcinoma).
Rule of
Clinical features
- Classic Triad (uncommon, <10% of pts, suggests advanced disease):
- Hematuria (most common presenting sign)
- Flank pain
- Palpable abdominal mass
- Many cases are found incidentally on imaging (CT/ultrasound).
- Can present with left-sided varicocele if tumor invades the left renal vein, blocking drainage of the left gonadal vein.
- Paraneoplastic Syndromes (Very High-Yield)
- “GREAT” mnemonic:
- Gonadotropin (hCG)
- Renin → Hypertension
- Erythropoietin (EPO) → Polycythemia
- ACTH → Cushing syndrome
- Tumor-associated Hypercalcemia (due to PTHrP)
- “GREAT” mnemonic:
Diagnostics
Pathology
Clear cell renal cell carcinoma
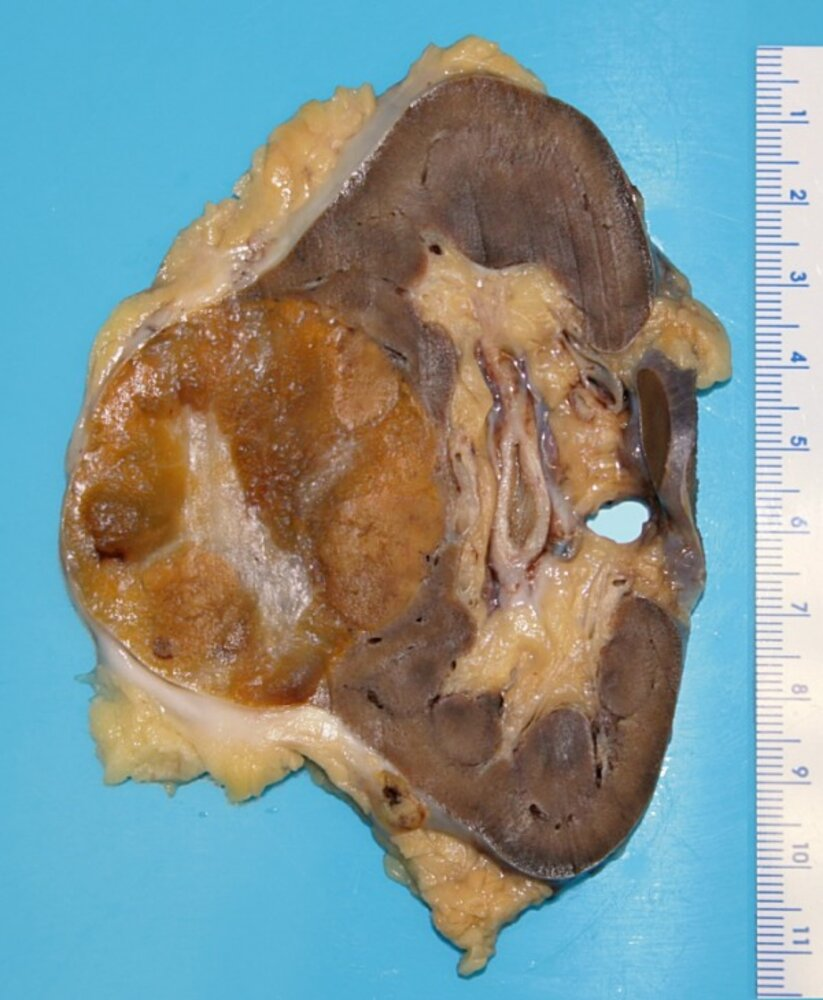
- Macroscopic appearance
- Yellow or golden due to high intracellular lipid concentration
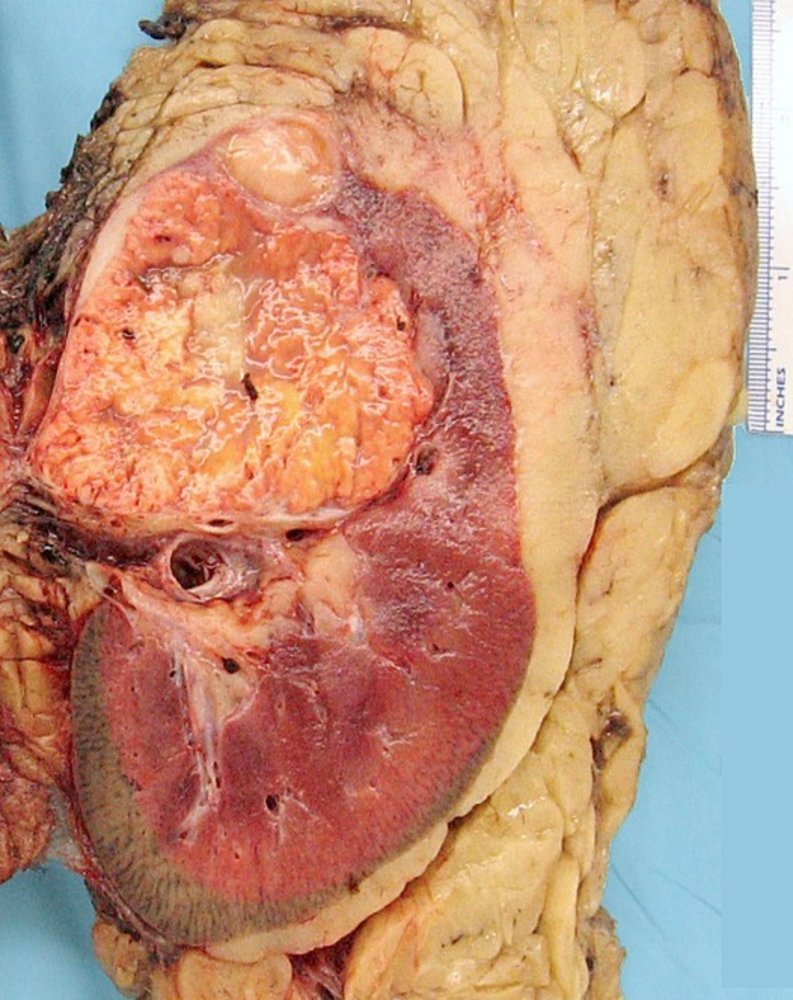
- Yellow or golden due to high intracellular lipid concentration
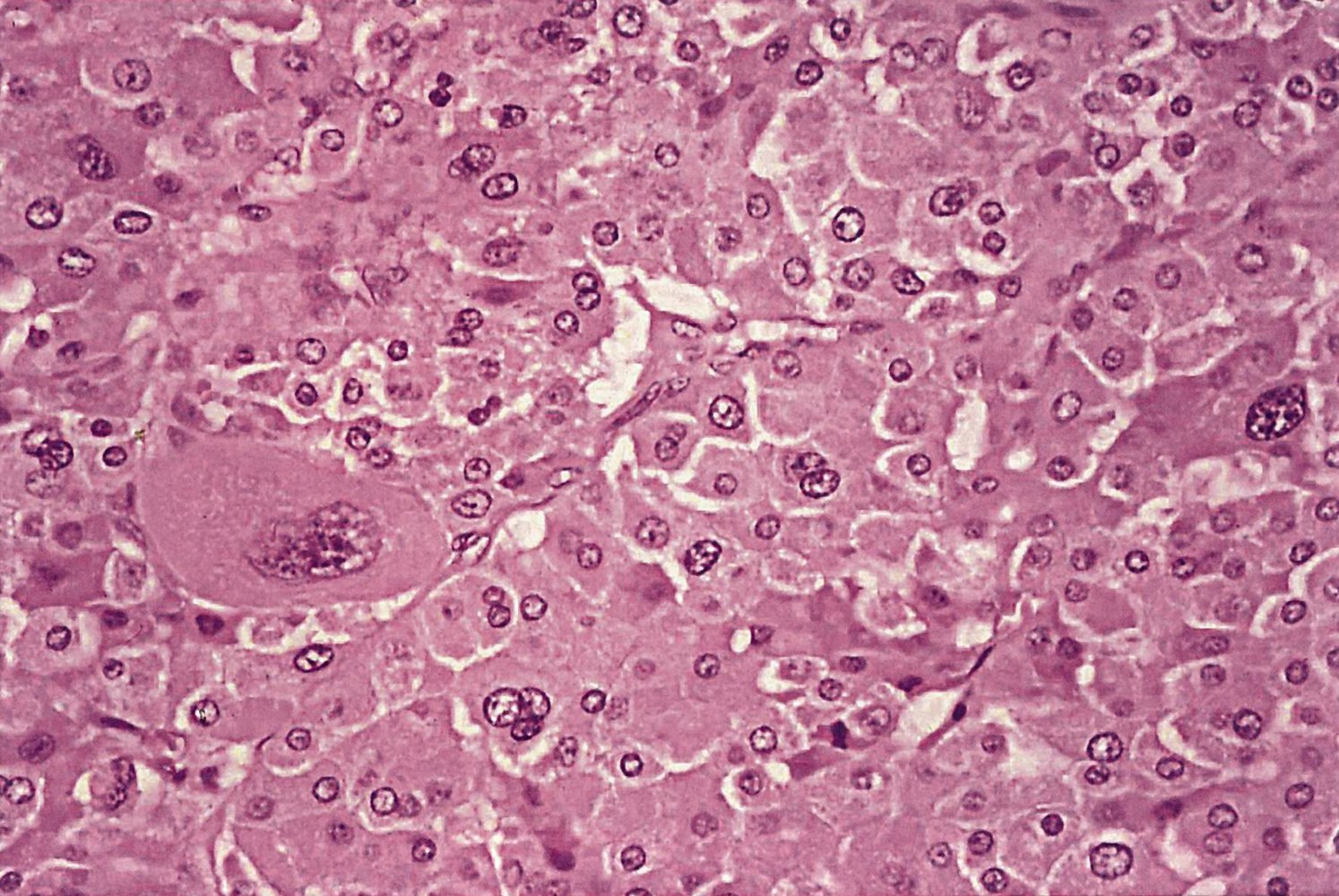
- Microscopic appearance
- Clear cells
- Polygonal cells arranged as cords or tubules (non-papillary growth)
- Clear, glycogen and/or lipid-filled cytoplasm
- Mutations in the VHL gene lead to accumulation of hypoxia-inducible factor (HIF).
- The accumulation of HIF promotes a cellular environment that mimics hypoxia (low oxygen levels), even when oxygen is abundant. This state triggers several metabolic changes in the cell, notably an increase in glucose uptake and a shift towards glycolysis and lipid biosynthesis. Consequently, lipids accumulate within the cytoplasm, giving the cells their characteristic “clear” appearance.
- Unifocal, unilateral growth
- Clear cells
Differential diagnosis
Benign renal masses
Oncocytoma
- Definition: benign epithelial tumor arising from the intercalated tubular cells in the collecting duct
Mnemonic
**collecting ducts, well-c**ircumscribed mass with central scar
- Clinical features
- Painless hematuria
- Abdominal mass
- Flank pain
- Pathology
- Macroscopy: smooth, clearly defined brown tumor with central radial scar
- Microscopy
- Large eosinophilic cells with abundant mitochondria without perinuclear clearing (Compared with chromophobe renal cell carcinoma)
- Excessive amount of mitochondria → acidophilic, granular cytoplasm without perinuclear clearing (unlike chromophobe RCC)
- Large eosinophilic cells with abundant mitochondria without perinuclear clearing (Compared with chromophobe renal cell carcinoma)
- Macroscopy: smooth, clearly defined brown tumor with central radial scar
- Treatment
- Often resected in order to exclude RCC
- Surveillance
Treatment
Complications
Complications caused by paraneoplastic syndromes
- Secondary hypercortisolism: due to ectopic ACTH release
- Secondary polycythemia: due to ectopic erythropoietin (EPO) secretion
- Hypertension: due to the release of renin
- Hypercalcemia: due to the release of PTHrP (parathyroid hormone-related protein)
Complications caused by local spread
- Varicocele
- Rare, classically associated with left-sided RCC
- Malignant cells grow inside the left renal vein and occlude the ostium of the left gonadal vein.
- Budd-Chiari syndrome: caused by involvement of the IVC
- Lower limb edema
- Ascites
- Hepatic dysfunction