Epidemiology
- Typical age of onset: bimodal distribution with one peak at 15–35 years and another one at 55–70 years
Tip
Compared with Ulcerative colitis, which peaks at 15-35 y/o.
- Populations with higher prevalence
- Individuals of Northern European descent
- Individuals of Ashkenazi Jewish descent
Etiology
- Risk factors
- Familial aggregation
- Genetic predisposition (e.g., mutation of the NOD2 gene, HLA-B27 association)
- Tobacco smoke
Tip
- Nicotine consumption is the only (known) controllable risk factor for CD. Therefore, smoking cessation is especially important in patients with CD.
- While smoking is a protective factor in Ulcerative colitis
Pathology
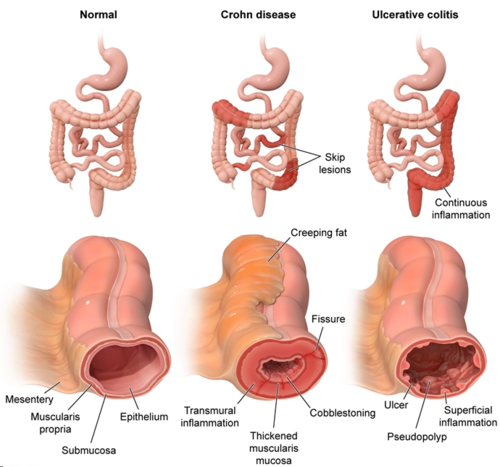
- Transmural inflammation: all mucosal layers of the intestinal wall are involved
- Noncaseating granulomas
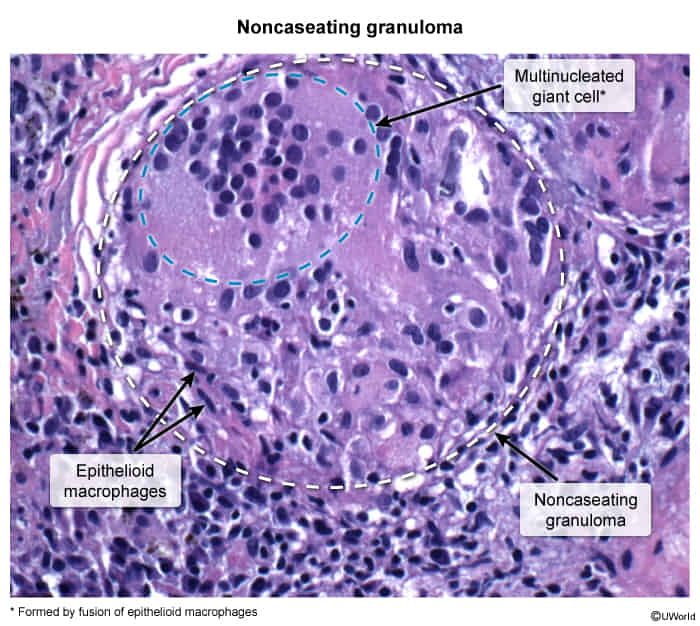
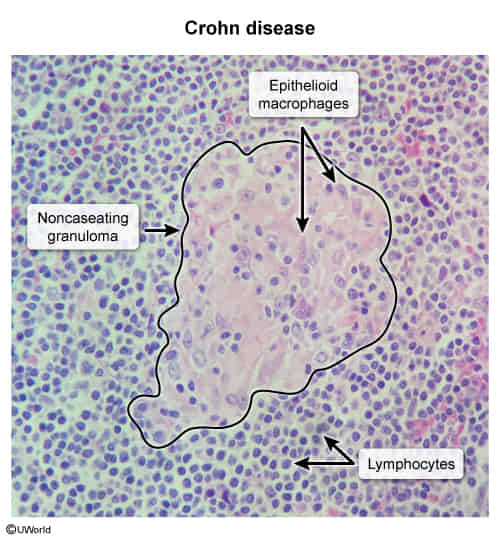
- Noncaseating granulomas
Clinical features
Constitutional symptoms
- Low-grade fever
- Weight loss
- Fatigue
Gastrointestinal symptoms
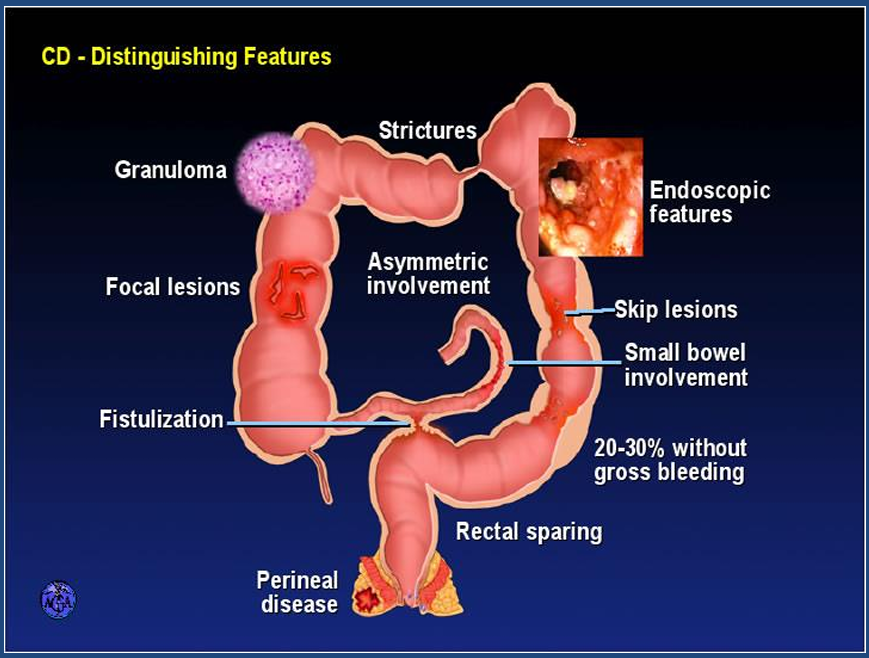
CD most commonly affects the terminal ileum and colon, but involvement of any part of the GI tract (from mouth to anus) is possible. In contrast to ulcerative colitis, rectal involvement is uncommon.
- Chronic diarrhea, typically nonbloody, watery
- Lower gastrointestinal bleeding (uncommon)
- microscopic (i.e., identified only on stool analysis) or overt
- Abdominal pain, typically in the RLQ
- Palpable abdominal mass in the RLQ
- Due to adhesions within the intestine caused by inflammation

- Due to adhesions within the intestine caused by inflammation
- Features of CD complications
- Malabsorption (e.g., weight loss, anemia, failure to thrive)
- Since ulcerative colitis does not affect the small intestine, absorption of nutrients is not impaired. However, loss of appetite, poor tolerance of or avoidance of certain foods, and adjustment of diet without medical consultation can lead to malnutrition already in nonsevere disease.
- Enterocutaneous or perianal fistulas, often associated with abscess formation
- Malabsorption (e.g., weight loss, anemia, failure to thrive)
Tip
Anemia in CD may result from chronic disease, iron deficiency, and/or vitamin B12 deficiency.
Extraintestinal symptoms
- Joints
- Enteropathic arthritis
- Eyes
- Uveitis
- Iritis
- Episcleritis
- Oral mucosa
- Oral aphthae
- Pyostomatitis vegetans
- Skin
- Erythema nodosum
- Acrodermatitis enteropathica
- Pyoderma gangrenosum: a neutrophilic dermatosis

- Associated with various conditions (e.g., IBD, rheumatoid arthritis, and trauma)
- Manifests with very painful, rapidly-progressive, red spots that can change into purulent pustules or deep ulcerated lesions with central necrosis
- Commonly located at extensor side of the lower limbs
- Treated with immunosuppressants (e.g., corticosteroids, cyclosporine A)
Diagnostics
Endoscopy
- Indication: all patients with suspected CD
- Assesses the distribution and severity of the disease
- Aids differentiation of CD from other diseases (e.g., ulcerative colitis)
- Monitors disease activity (e.g., active disease, remission)
- Can be used therapeutically (e.g., stricture dilatation)
- Supportive findings
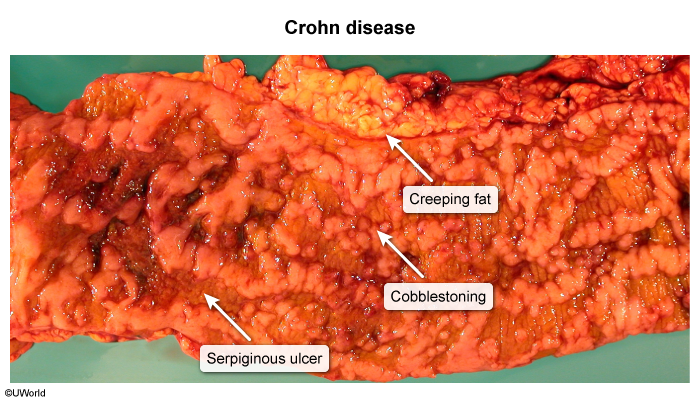
- Skip lesions: segmental and/or discontinuous pattern of involvement (interspersed with normal tissue)
- Linear and/or serpiginous ulcerations
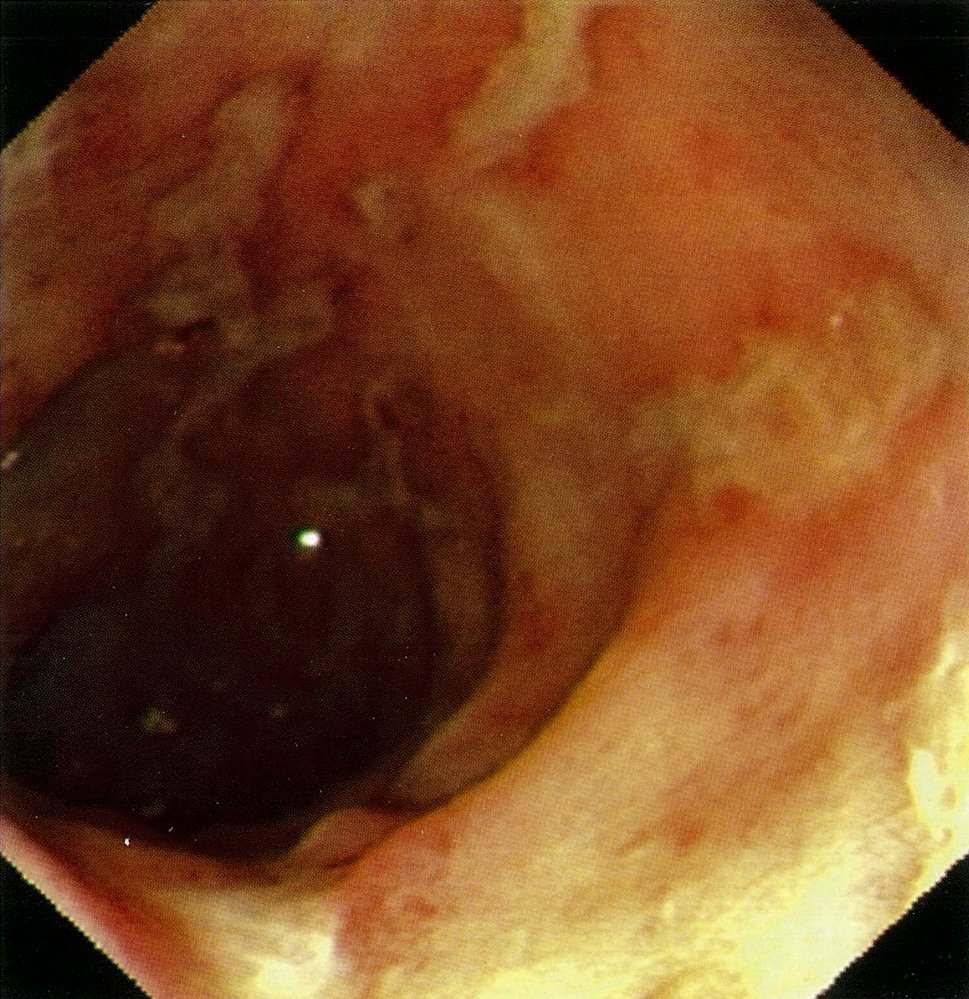
- Small aphthous ulcerations
- Cobblestone sign: inflamed edematous sections interspersed with deep ulcerations that resemble cobblestones

- Erythema, fissures, strictures, and fistulas
Imaging
- Cross-sectional enterography (MRE, CTE): preferred imaging modality for CD
- Edematous thickening of the intestinal wall
- Creeping fat: excessive mesenteric fat around the affected segments of bowel
- Possibly in response to intestinal bacteria translocation
Laboratory studies
- To monitor disease activity
- Fecal calprotectin and/or fecal lactoferrin: proteins associated with neutrophil activation
- Used as noninvasive markers of intestinal inflammation to monitor disease activity and response to therapy
- Also used to differentiate IBD from irritable bowel syndrome
- Inflammatory markers: CRP, ESR
- Fecal calprotectin and/or fecal lactoferrin: proteins associated with neutrophil activation
Treatment
Principle
- Induction phase
- Used to manage acute flares.
- Agents that have a rapid onset of action (e.g., corticosteroids, biologics) are used.
- Maintenance phase
- Used to maintain remission, typically in patients with moderate or severe CD and those at high risk of progression of CD.
- Biologics and immunomodulators are the principal agents of maintenance therapy.
Pharmacotherapy
- Corticosteroids
- Primarily used to induce remission
- Agents used (depending on severity of CD):
- Controlled ileal release budesonide
- A formulation of the synthetic steroid budesonide that is released in environments with a pH ≥ 5.5, which facilitates drug delivery distal to the proximal small bowel
- Used to treat Crohn disease that involves sites of inflammation in the ileum and/or ascending colon
- Controlled ileal release budesonide
- Oral prednisolone
- IV methylprednisolone
- Biologics
- Anti-TNF-α antibodies: e.g., adalimumab, infliximab, certolizumab
- Increasingly used as a primary agent to induce remission.
- Also used to maintain remission and manage CD refractory to immunomodulators
- Anti-leukocyte trafficking antibody (vedolizumab) and anti-p40 antibody (ustekinumab) : used mainly to induce and maintain remission in moderate to severe CD
- Anti-TNF-α antibodies: e.g., adalimumab, infliximab, certolizumab
- Immunomodulators: e.g., thiopurine analogs (azathioprine, 6-mercaptopurine), methotrexate
- Primarily used to maintain remission
- Can be used as a steroid-sparing regimen to induce remission
- 5-aminosalicylic acid derivative: sulfasalazine (mesalamine is not routinely recommended)
- May be considered to induce remission of mild to moderate colonic or ileocolonic CD
- Not effective in isolated small bowel disease
Complications
Fistulizing CD
- Occur in one-third of patients with CD
- Typically involve the perianal region
Other intestinal complications
- Colorectal cancer (especially in the case of pancolitis)
- Short bowel syndrome and associated issues after surgery
- Stenosis/strictures → bowel obstruction/(sub)ileus
- Occur as a result of bowel wall edema, fibrosis, and hypertrophy (thickening) of the muscularis mucosae, which narrows the intestinal lumen
- Intestinal perforation → peritonitis
- Primary sclerosing cholangitis
- Impaired bile acid reabsorption
- Cholesterol gallstones
.jpg)
- Bile acid diarrhea
- Bile acid malabsorption → steatorrhea and deficiencies in fat-soluble vitamins
- Cholesterol gallstones
- Abscess formation/phlegmons
Systemic complications
- Signs of malabsorption syndrome
- Weight loss
- Failure to thrive and growth failure in children
- Anemia
- Iron deficiency anemia
- Caused by intestinal blood loss
- Megaloblastic anemia (vitamin B12 deficiency due to impaired absorption in the chronically inflamed ileum)
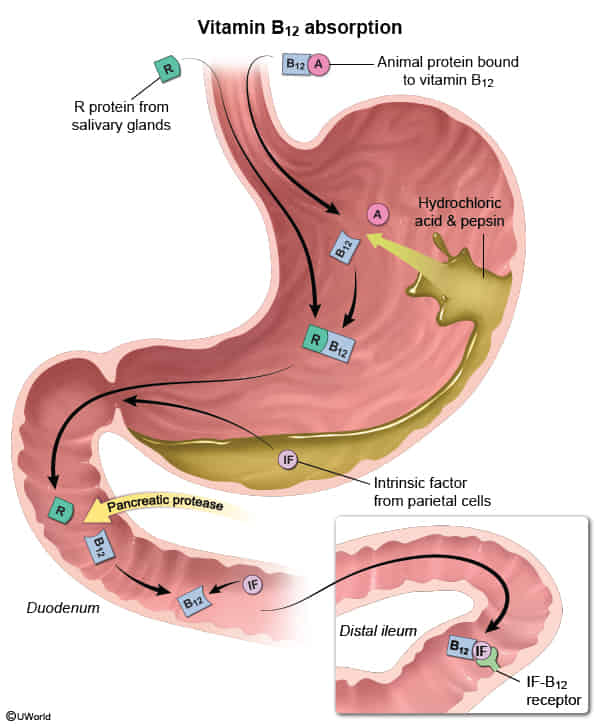
- Iron deficiency anemia
- Osteoporosis