Etiology
Three classifications, same as Nephritic syndrome > Etiology
Pathophysiology
- Breaks in the glomerular capillary wall and dysfunction of the glomerular basement membrane (GBM) → leakage of plasma proteins (e.g., coagulation factors) and passage of inflammatory cells (macrophages, T cells) into Bowman space
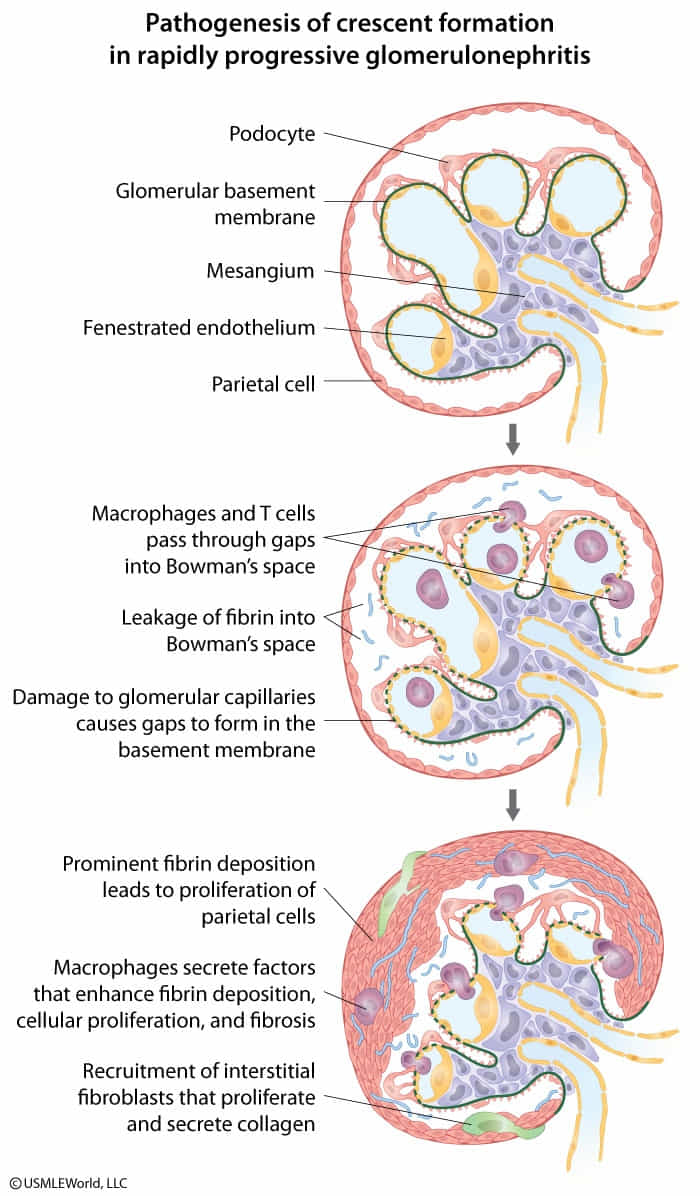
- Release of inflammatory cytokines → damage to the membrane of Bowman space and passage of cells from the interstitium into Bowman space
- This causes the formation of fibrin clots and proliferation of cells (e.g., macrophages, fibroblasts, neutrophils, epithelial cells) → crescent moon formation → compression of the glomerulus → renal dysfunction
Clinical features
Diagnostics
- Antiglomerular basement membrane (anti-GBM) RPGN: Linear GBM deposits of IgG and C3 are found on immunofluorescence. In some patients, anti-GBM antibodies cross-react with pulmonary alveolar basement membranes, producing pulmonary hemorrhages (Goodpasture syndrome).
- Immune-complex RPGN: There is a “lumpy-bumpy” granular pattern of staining for both antibodies (eg, IgG, IgA) and complement on immunofluorescence microscopy. This can be a complication of poststreptococcal glomerulonephritis, systemic lupus erythematosus, IgA nephropathy, or Henoch-Schönlein purpura.
- Pauci-immune RPGN: There are no immunoglobulin or complement deposits on the basement membrane. Most patients have elevated serum titers of ANCA. This condition is often associated with vasculitides (eg, granulomatosis with polyangiitis, microscopic polyangiitis) but can also be idiopathic.
Treatment
<% tp.file.cursor() %>