Epidemiology
- Diabetic polyneuropathy is the most common form of polyneuropathy in high-income countries.
Etiology
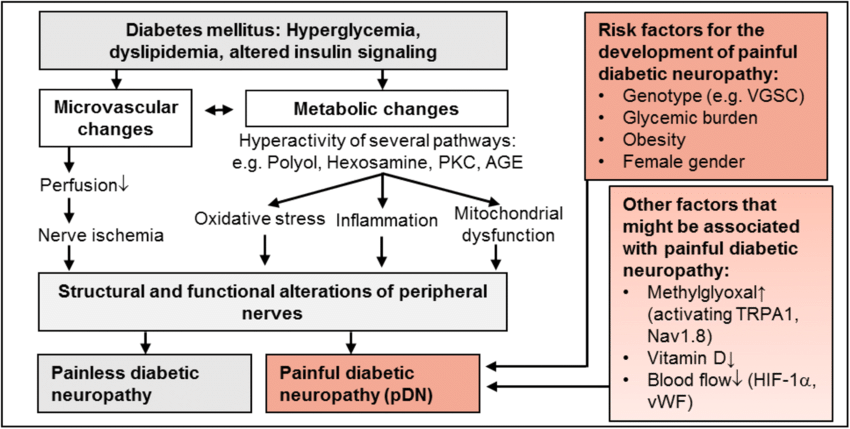
Pathophysiology
- Caused by nerve ischemia and metabolic damage (e.g. oxidative stress, inflammation)
- Symptoms vary depending on the type of nerve fibers involved:
- Small-fiber injury is characterized by predominance of positive symptoms (eg, pain, paresthesias, allodynia).
- Large-fiber involvement is characterized by predominance of negative symptoms (eg, numbness, loss of proprioception and vibration sense, sensory ataxia (eg, positive Romberg sign), diminished ankle reflexes).
Clinical features
Diabetic peripheral neuropathy
- Sensory symptoms
- Distal symmetrical sensory loss: stocking glove sensory loss pattern with proximal progression
- Numbness
- Tingling
- Dysesthesia (e.g., burning feet syndrome with symptoms that worsen at night)
- Motor weakness: e.g., ataxia, balance issues
- Motor findings are late manifestations of the condition.
- Neurological examination may show loss or reduction of:
- Vibration sense (using a tuning fork)
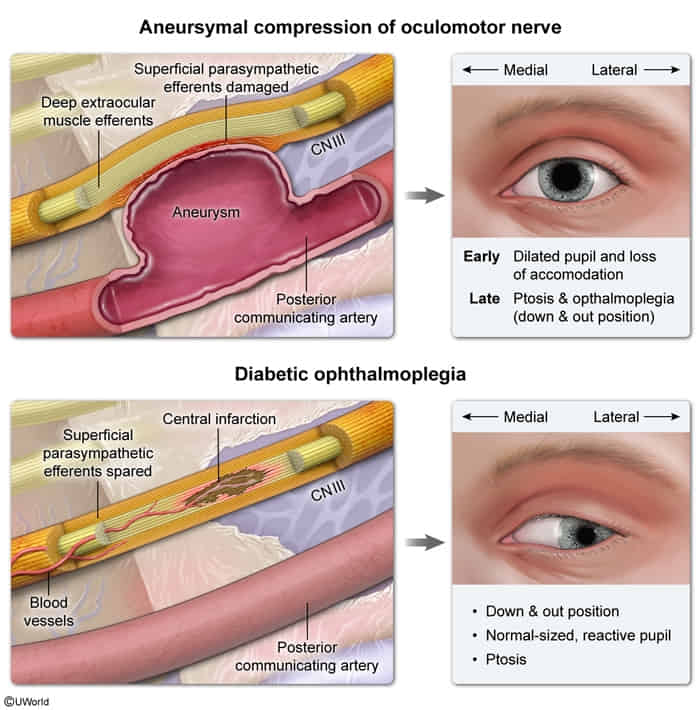
Diabetic CN III mononeuropathy
- Diabetic CN III mononeuropathy classically presents with acute onset diplopia.
- On examination, the affected eye assumes a “down and out” position due to the unopposed pull by the superior oblique (CN IV) and lateral rectus (CN VI) muscles because all other extraocular muscles (inferior oblique and superior, inferior, and medial recti) are supplied by CN III. Ptosis also occurs due to paralysis of the levator palpebrae.
- Diabetic mononeuropathy is caused by ischemic nerve damage, which predominantly involves the core of the CN III with relative sparing of the peripheral part. The somatic component of CN III that innervates the extraocular muscles is located centrally, but the autonomic component responsible for pupillary constriction and accommodation is located in the peripheral aspect of the nerve. Therefore, pupillary size and reactivity is normal in diabetic CN III mononeuropathy.
Diabetic autonomic neuropathy
Gastrointestinal autonomic neuropathy
- Painless, watery diarrhea
- Secretory-like (persists at night & while fasting)
- Laboratory evaluation typically unremarkable
Genitourinary autonomic neuropathy
- Sexual dysfunction (e.g., erectile dysfunction)
- Neurogenic bladder, e.g.:
- Urinary retention
- Incomplete bladder emptying
- Bladder distention
- Overflow incontinence
- Poor urinary stream
Cardiovascular autonomic neuropathy
- Early: decreased heart variability
- Late:
- Orthostatic hypotension
- Tachycardia at rest
- due to unopposed sympathetic nerve activity
Warning
Patients with cardiovascular autonomic neuropathy are at increased risk for silent myocardial infarction, arrhythmias, and death.
Other autonomic neuropathies
- Impaired pupillary tone