Etiology
- Atrial remodeling due to:
- Age-related myocardial changes
- Atrial enlargement from heart disease (eg, HTN, MS)
- Foci of rapid electrical activity:
- Commonly originate in pulmonary veins
- Alcohol intake & ↑ sympathetic drive may contribute
Pathophysiology
- The new onset of Afib triggers a vicious circle that can ultimately lead to long-standing Afib with atrial remodeling:
- Afib is triggered by one or both of the following
- Bursts of electrical activity from automatic foci near the pulmonary vein ostia (left atrium) or in diseased, fibrotic atrial tissue
- Pre-excitation of the atria as a result of aberrant pathways (e.g., WPW syndrome)
- Afib is sustained by re-entry rhythms and/or rapid focal ectopic firing
- Re-entry rhythms are more likely to occur with enlarged atria, diseased heart tissue, and/or aberrant pathways (e.g., WPW syndrome).
- Atrial remodeling
- Electrophysiological changes in the atria occur within a few hours of Afib onset (electrical modeling).
- If Afib persists, atrial fibrosis and dilatation (structural remodeling) occur within a few months.
- Electrical and structural remodeling increase susceptibility to Afib, resulting in a vicious circle.
- Afib is triggered by one or both of the following
- Effects of Afib
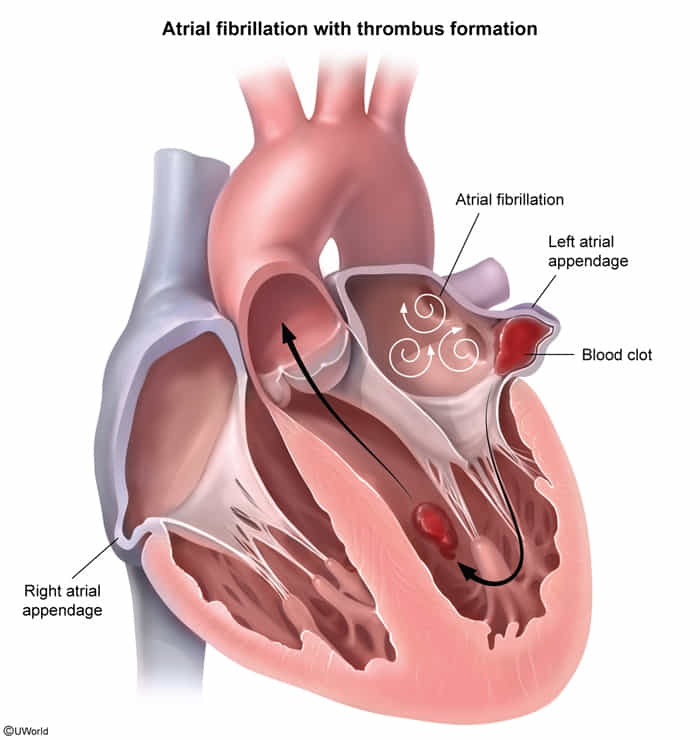
- The atria contract rapidly but ineffectively and in an uncoordinated fashion → stasis of blood within the atria, especially in atrial appendage → risk of thromboembolism and stroke
- Irregular activation of the ventricles by conduction through the AV node → tachycardia
- The atria contract rapidly but ineffectively and in an uncoordinated fashion → stasis of blood within the atria, especially in atrial appendage → risk of thromboembolism and stroke
Clinical features
Diagnostics
Atrial flutter vs atrial fibrillation
Link to original
Feature Atrial Flutter Atrial Fibrillation Site of Origin Right Atrium (re-entrant circuit involving the cavotricuspid isthmus). Left Atrium (ectopic foci, most commonly near the pulmonary vein ostia). Pathophysiology Organized macro-reentrant circuit. Chaotic multiple atrial foci. ECG Rhythm Regular or regularly irregular. Irregularly irregular. Atrial Waves (ECG) “Sawtooth” flutter waves (~300 bpm). Fibrillatory waves (no P waves). Management Pearl Catheter ablation is highly curative. Lifelong anticoagulation (CHA₂DS₂-VASc score) is key to prevent stroke.
ECG
QRS complex
- Typically narrow QRS complex (< 0.12 seconds)
- Wide QRS complex may be seen in some situations:
- Aberrant conduction, e.g., bundle branch block or preexcitation (as seen in Afib with WPW)
- Complete AV block with a ventricular escape rhythm
- Ashman phenomenon: intermittent aberrant ventricular conduction results in isolated or short runs of wide QRS complexes

Warning
Wide QRS complex may indicate preexcited Afib or aberrant conduction.
Treatment
- First-line
- Beta blockers: e.g., metoprolol, atenolol, propranolol
- Via blockade of sympathetic tone
- Work well both during rest and exercise
- Preferred when Afib is due to hyperthyroidism and in pregnant patients
- Avoid in patients with COPD and acute decompensated heart failure (ADHF).
- OR nondihydropyridine calcium channel blockers (ndHP CCBs): e.g., diltiazem, verapamil
- Work well both during rest and exercise
- Avoid in patients with ADHF.
- Can be safely used in heart failure with preserved normal LV systolic function.
- Beta blockers: e.g., metoprolol, atenolol, propranolol
- Second-line: digoxin; preferred initial therapy for patients with ADHF
- Via increased parasympathetic tone
- This mechanism is effective at rest, when sympathetic tone is low, but it poorly controls ventricular rate during exercise, when high levels of sympathetic tone accelerate AV node conduction. t
- Third-line: amiodarone; typically reserved for patients in whom all other options have failed