Epidemiology
- Incidence
- Second most common gynecological cancer (after endometrial cancer)
- Incidence increases with age
- Age
- Peak incidence: 55–64 years of age
Etiology
The most likely pathogenesis of EOC is repeated injury and repair to the ovarian surface, which makes surface epithelial cells susceptible to malignant transformation (ie, acquiring oncogenic mutations).
Risk factors
- Hormonal factors
- Elevated number of ovulatory cycles: early menarche and/or late menopause
- Nulliparity
- Endometriosis
Protective factors
- Combined oral contraceptive pills
- Multiparity
- Breastfeeding
- Bilateral salpingo-oophorectomy
- Bilateral tubal ligation
- Hysterectomy
Pathophysiology
- BRCA1/BRCA2 mutations: ↑ lifetime risk to 40-50%
- Lynch syndrome (HNPCC): ↑ risk of endometrial and ovarian cancer
- Incessant ovulation hypothesis: ↑ ovulations → ↑ epithelial damage → ↑ malignancy risk
- Protective factors: Multiparity, breastfeeding, OCPs (↓ ovulations)
Clinical features
Tip
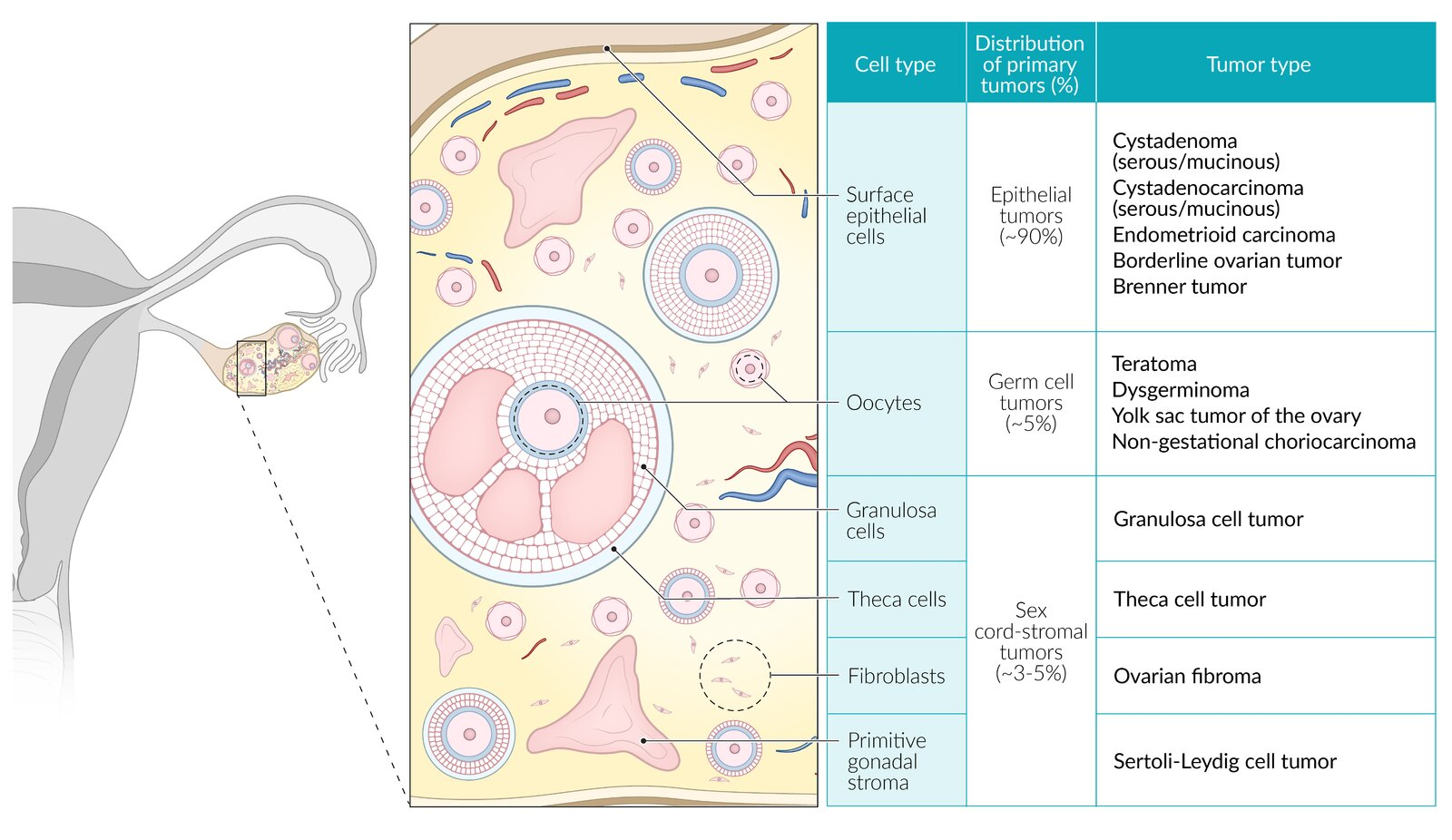
- Surface epithelial-stroma: composed of cells that support the normal ovarian structure for ovulation (eg, serous, mucinous epithelial cells).
- Germ cell: composed of cells that can develop into an embryo or placenta. These tumors are composed of varying amounts of germ layers (ie, endoderm, mesoderm, ectoderm), yolk sac, or placenta (eg, chorion). They often have associated hormonal activity (eg, increased hCG, alpha fetoprotein).
- Sex cord-stroma: composed of cells that support and surround the oocyte. These cells secrete sex hormones including estrogen (granulosa cells) and testosterone (Sertoli-Leydig cells).
| Histologic type | Diagnosis | Key features |
|---|---|---|
| Epithelial | Serous cystadenocarcinoma | Most common ovarian cancer Often bilateral Histology: psammoma bodies |
| Mucinous cystadenocarcinoma | Pseudomyxoma peritonei Mucin-producing epithelial cells | |
| Germ cell | Dysgerminoma | Adolescents ↑ β-hCG, ↑ LDH Histology: “fried-egg” cells |
| Endodermal sinus (yolk sac) | ↑ AFP Aggressive Schiller-Duval bodies resembling glomeruli | |
| Stroma (sex cord) | Granulosa cell tumor | ↑ Estrogen (e.g., endometrial hyperplasia, postmenopausal bleeding) ↑ Inhibin Histology: Call-Exner bodies, coffee-bean nuclei |
| Sertoli-Leydig cell tumor | ↑ Androgens (e.g., hirsutism, clitoromegaly) |
Ovarian germ cell tumors
Epithelial ovarian tumors
Cystadenoma
- Ovarian serous cystadenoma and Ovarian mucinous cystadenoma
- Most (serous) and second most common (mucinous) benign ovarian tumor
- Histology
- Ovarian serous cystadenoma
- May contain small papillary projections
- Psammoma bodies
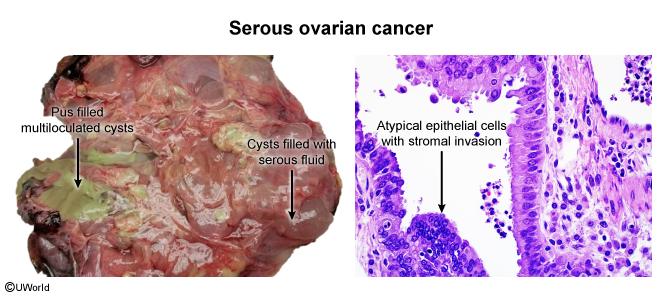
- Cyst is lined by serous epithelial cells (similar to the epithelium of fallopian tubes)
- Ovarian mucinous cystadenoma
- Cyst is lined by columnar epithelium that secretes thick mucus (similar to the epithelium of cervix)
- Ovarian serous cystadenoma
Ovarian germ cell tumors
- Subtypes are determined by structural differentiation
- Extraembryonic differentiation: yolk sac tumor
- Somatic differentiation: teratoma
- No differentiation: dysgerminoma
Diagnostics
Tumor markers
- CA-125: Elevated in >80% of epithelial ovarian cancers. Best used for monitoring treatment response, not for screening (low specificity, can be elevated in endometriosis, PID, fibroids).
- Why it’s elevated: CA-125 (Cancer Antigen 125) is a glycoprotein expressed on the surface of coelomic epithelium, from which most epithelial ovarian cancers derive.
- Germ Cell Tumors: ↑ hCG (Choriocarcinoma, Dysgerminoma), ↑ AFP (Yolk Sac/Endodermal sinus tumor), ↑ LDH (Dysgerminoma).
- Choriocarcinoma is a malignant tumor of syncytiotrophoblasts and cytotrophoblasts, the same cells that form the placenta. A primary function of placental syncytiotrophoblasts is to produce hCG to maintain the corpus luteum during pregnancy.
- Yolk sac tumor is composed of cells that differentiate to resemble the embryonic yolk sac. During early fetal development, the yolk sac is the primary producer of AFP.
- Dysgerminomas are composed of undifferentiated germ cells and are characterized by very rapid growth and cell turnover. LDH is an intracellular enzyme involved in anaerobic glycolysis. High cell turnover and cell death (necrosis) lead to the release of large amounts of LDH into the circulation.
- Sex Cord-Stromal: ↑ Inhibin and estrogen (Granulosa cell tumor), ↑ testosterone (Sertoli-Leydig cell tumor)
- This tumor is composed of malignant granulosa cells. In a normal menstrual cycle, granulosa cells surround the oocyte within the follicle and produce inhibin to provide negative feedback to the pituitary gland, suppressing FSH secretion. They also produce estrogen. A tumor of these cells retains this function, leading to high circulating levels of inhibin A and B, which serves as an excellent tumor marker. The excess estrogen can cause endometrial hyperplasia or precocious puberty.