Epidemiology
Etiology
Bacterial
- Neisseria meningitidis (First peak: < 2 years of age; second peak: 16–20 years of age)
- Streptococcus pneumoniae (most common in adults >20 and elders)
Most common causative agents of bacterial meningitis by age group and underlying condition
- Immunocompromise
- Listeria monocytogenes
- Streptococcus pneumoniae
- Haemophilus influenzae type b
- Gram-negative bacilli (e.g., Escherichia coli, Salmonella spp.)
Other etiologies
- Viral meningitis: often associated with encephalitis (meningoencephalitis)
- Enteroviruses (especially coxsackieviruses and echoviruses): the most common cause of all types of meningitis in all patient groups
- Herpesviruses: HSV (meningitis is more commonly caused by HSV2 than HSV1)
Pathophysiology
Pathways of infection
- Most pathogens that cause meningitis colonize the nasopharynx or the upper airways before entering the CNS via:
- Hematogenous dissemination
- About 5–10% of the US adult population are colonized with Neisseria meningitidis. The bacteria attach to the nasopharyngeal mucosa, where they can persist for long periods of time. Hematogenous dissemination may then occur subsequent to mucosal infiltration facilitated by infection with another pathogen capable of infiltrating the mucosa, e.g., adenovirus.
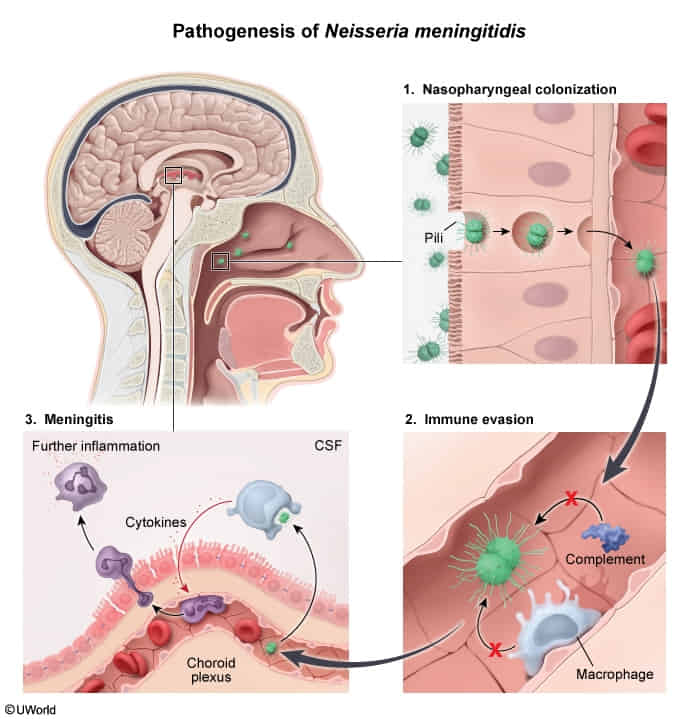
- About 5–10% of the US adult population are colonized with Neisseria meningitidis. The bacteria attach to the nasopharyngeal mucosa, where they can persist for long periods of time. Hematogenous dissemination may then occur subsequent to mucosal infiltration facilitated by infection with another pathogen capable of infiltrating the mucosa, e.g., adenovirus.
- Contiguous spread of infections in nose, eyes, and ears
- Retrograde transport along or within peripheral or cranial nerves
- E.g. Naegleria fowleri via CN I, see below
- Direct infection (e.g., due to trauma or head surgery)
- Hematogenous dissemination
Subtypes and variants
Primary amebic meningoencephalitis
- Pathogen: Naegleria fowleri (colloquially referred to as “brain-eating amoeba”), found in warm freshwater (e.g., ponds, hot springs)
- Route of infection: via contaminated water entering the nose (e.g., while swimming) → invades the CNS directly via the olfactory nerve (perforates the cribriform plate)
- Clinical features: causes fulminant meningoencephalitis with rapid onset
- Diagnosis
- CSF analysis
- Findings similar to those of bacterial meningitis (e.g., neutrophilic pleocytosis, hypoglycorrhachia, increased CSF protein)
- CSF erythrocytosis (due to hemorrhagic necrosis)
- Microscopy shows trophozoites
- CSF analysis
- Treatment: amphotericin B, miltefosine
- Prognosis: nearly always fatal
Clinical features
Diagnostics
Differential diagnostics
| Feature | Meningitis | Meningo-encephalitis | Encephalitis |
|---|---|---|---|
| Fever, leukocytosis | Often | Often | Often |
| Meningeal irritation (e.g. Nuchal rigidity, photophobia) | Often | Often | No |
| Mental status alteration | Sometimes | Often | Nearly always |
| Seizure | Uncommon | More often than in meningitis | Often |
| Focal neurologic findings | Half of patients develop focal findings at some point during the disease course (usually later) | More often than in meningitis | Hallmark feature |
| Typical pathogens | Streptococcus pneumoniae, N. meningitidis, H. influenzae | HSV, VZV, Listeria spp. | HSV, VZV, Enteroviruses |
| *Focal neurologic findings include weakness, visual disturbance, [[aphasia | aphasia]], cerebellar findings, behavior change |
Treatment
Prevention
N. meningitidis
- Indications
- All close contacts within 7 days of symptom onset, i.e.:
- Household members
- All close contacts within 7 days of symptom onset, i.e.:
- Recommended regimens
- Rifampin
- OR ceftriaxone
H. influenzae
- Rifampin for 4 days