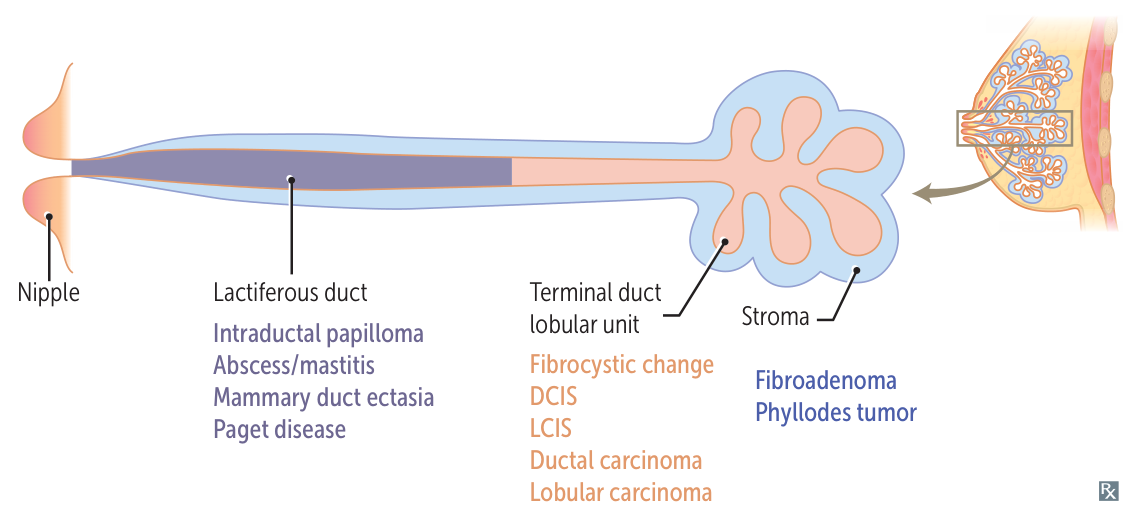
Breast anatomy
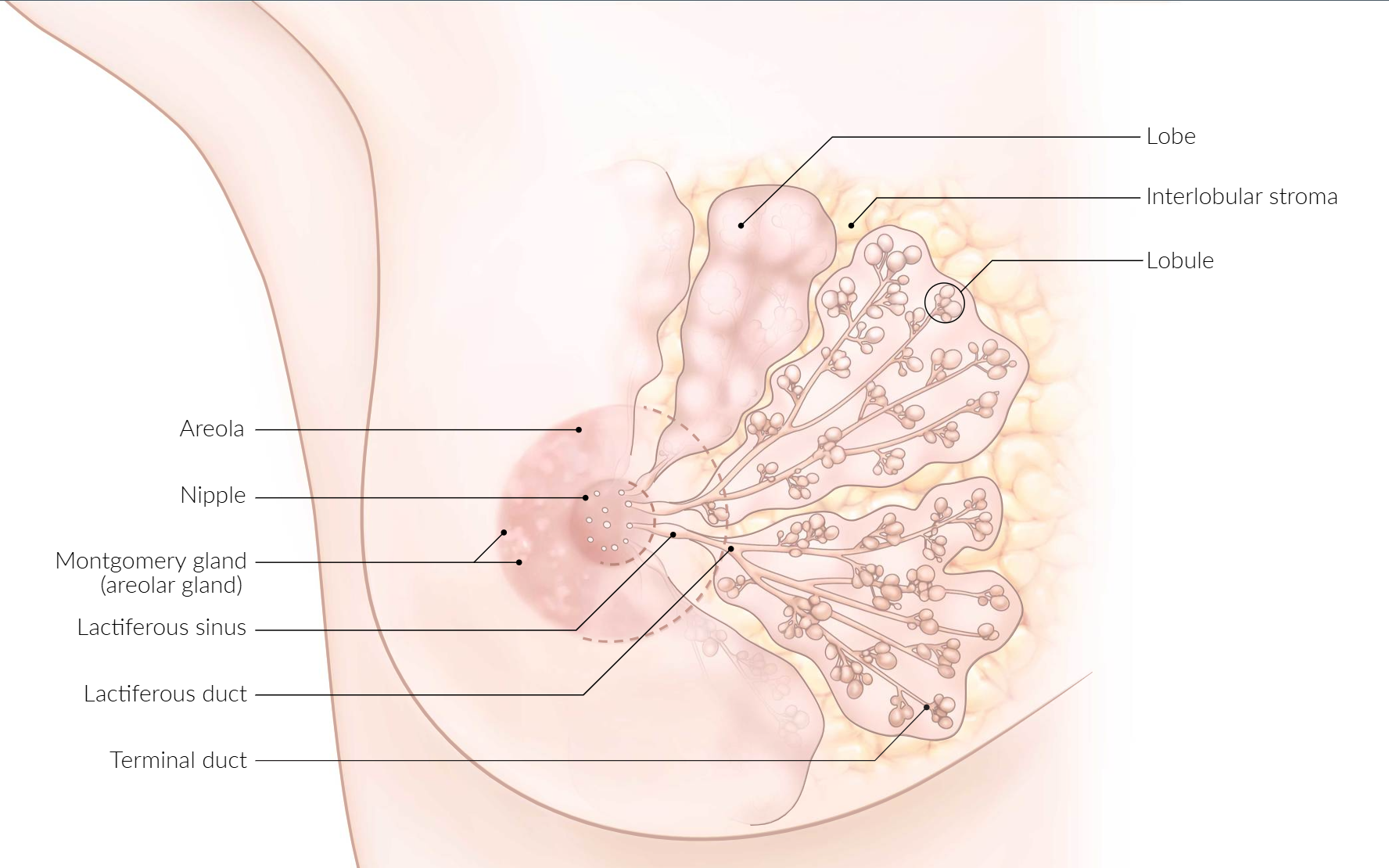
- Terminal ductal lobular units (TDLU)
- Basic histopathological units of the mammary gland
- Consist of:
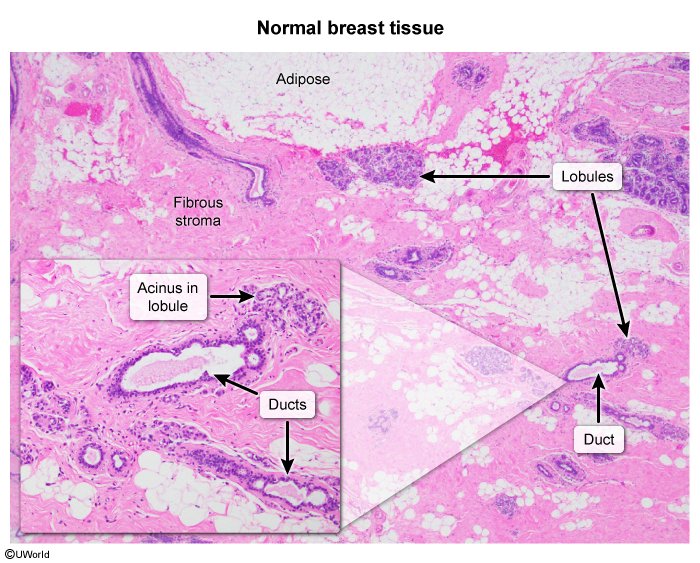
- Lobule of the mammary gland: (functional unit of the breast)
- Intralobular stroma: loose, cell-rich connective tissue
- Intralobular terminal (milk) duct with multiple outpouchings called acini or ductules (site of milk production)
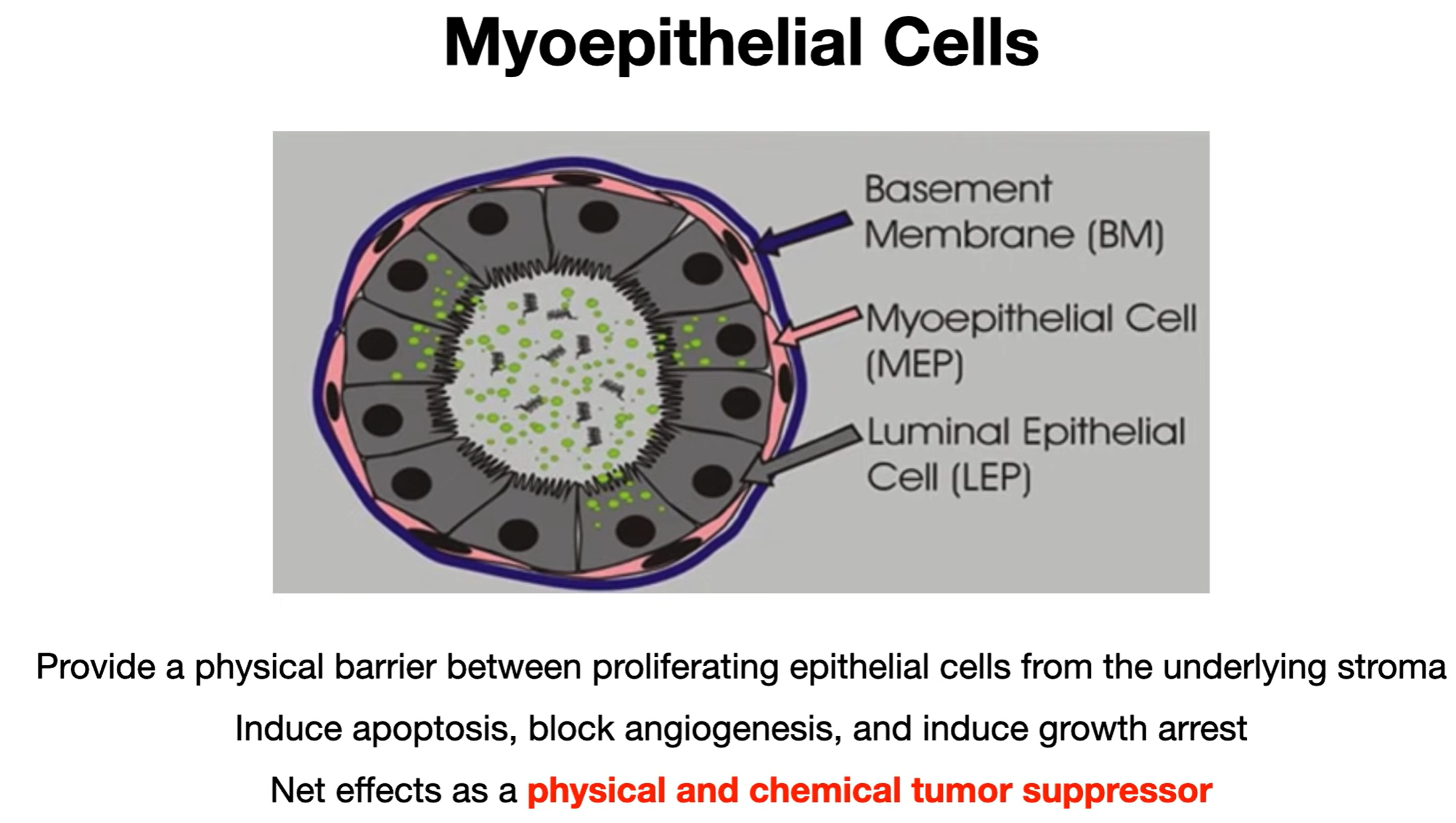
- Structure: tubulo-alveolar with two-layered glandular epithelium
- Outer layer: myoepithelial cells (contractile, route the milk to the ducts in lactating breasts)
- Inner layer: cubic, apocrine glandular epithelial cells (can produce milk)
- Structure: tubulo-alveolar with two-layered glandular epithelium
- Extralobular terminal duct
- Lobule of the mammary gland: (functional unit of the breast)
Overview
Benign Breast Disease
- Fibrocystic Changes: Premenopausal. Cyclical, bilateral pain and lumps. No ↑ cancer risk.
- Fibroadenoma: Women <35. Firm, mobile, painless “breast mouse.” Estrogen sensitive. Benign.
- Intraductal Papilloma: Most common cause of unilateral bloody/serosanguineous nipple discharge.
- Atypical Hyperplasia: Highest risk factor among benign diseases for developing invasive carcinoma.
- Fat Necrosis: Hx of trauma. Can present as a fixed mass with calcifications, mimicking cancer.
- Acute Mastitis: During breastfeeding. S. aureus. Presents as a warm, erythematous, painful breast. Tx: Dicloxacillin, continue breastfeeding.
Malignant Breast Disease
- Ductal Carcinoma In Situ (DCIS)
- Non-invasive. Basement membrane intact.
- Often detected as microcalcifications on mammography.
- Paget Disease of the Breast
- Eczematous rash and ulceration of the nipple.
- Associated with underlying DCIS or invasive cancer.
- Invasive Ductal Carcinoma (IDC)
- Most common type of breast cancer (~80%).
- Presents as a hard, fixed, irregular mass.
- Invasive Lobular Carcinoma (ILC)
- Cells arranged in a single-file “Indian file” pattern.
- Due to loss of E-cadherin. Often bilateral.
- Inflammatory Breast Cancer
- Red, swollen, warm breast (“peau d’orange”).
- Caused by cancer cells in dermal lymphatics. Very aggressive.
Tip
Nipple discharge happens in duct-related diseases, or diseases affecting the nipple skin. It doesn’t happen in lobule-related diseases, or stromal cancer.
Benign cancer
Intraductal papilloma
- BIoody nipple discharge in pre-menopausal women (vs. Papillary Carcinoma)
- FibrovascuIar projections lined by luminal myoepithelial cells (vs. Papillary Carcinoma)
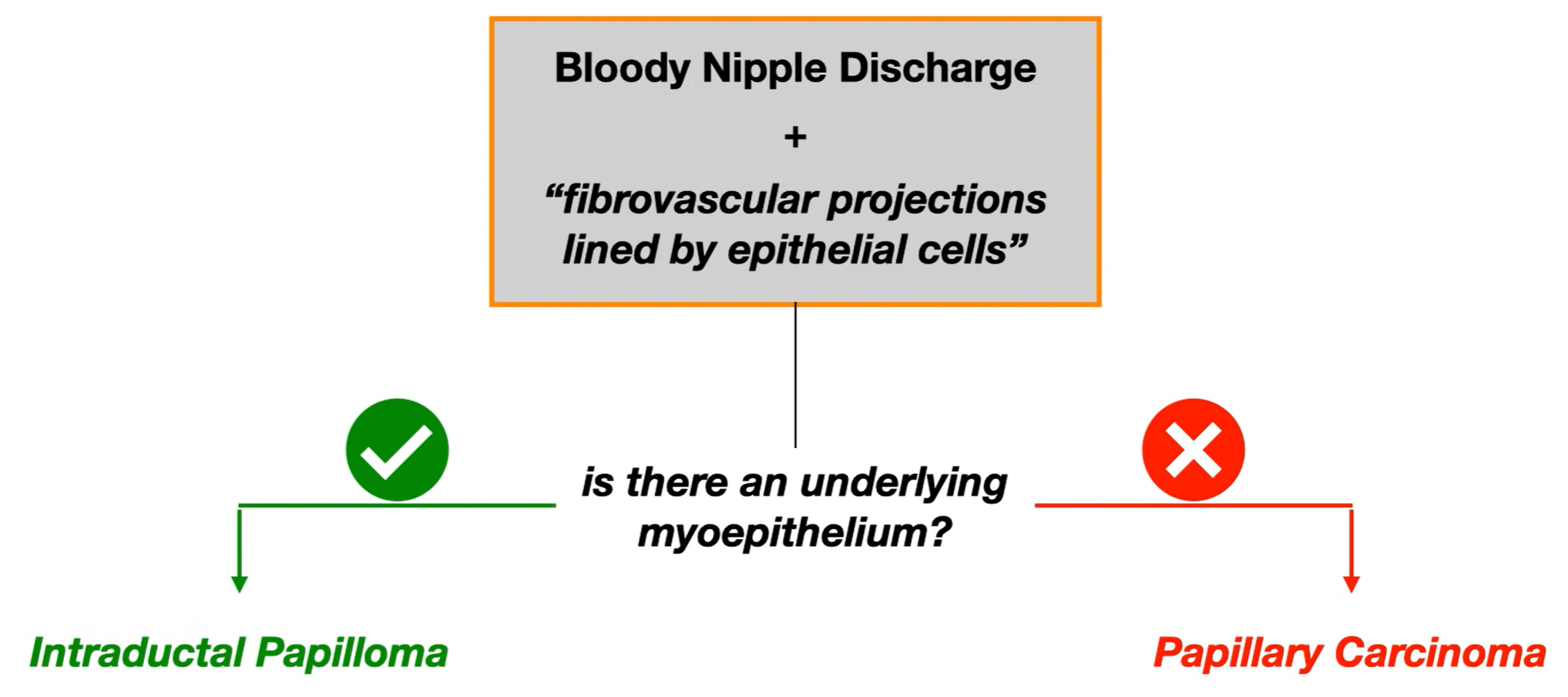
Mnemonic
- Intraductal = Myoepithelium Included
- Papillary = Myoepithelium Popped
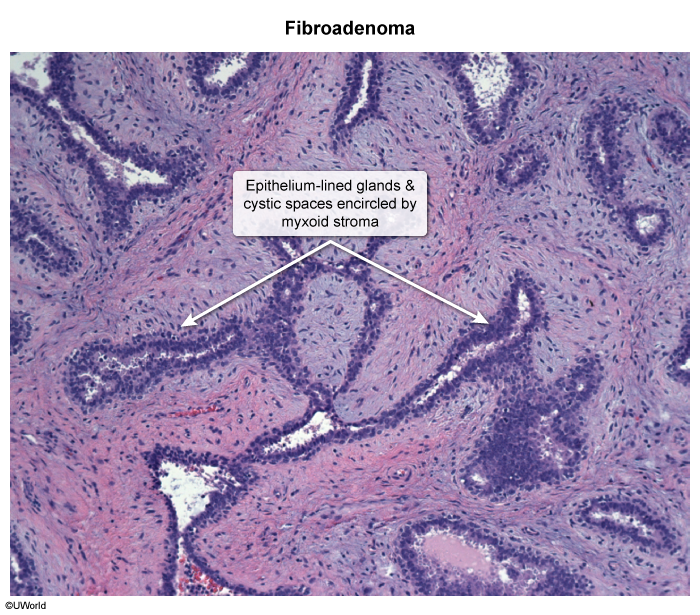
Fibroadenoma
- Refers to a marble-like, rubbery mobile, stromal/glandular benign tumor
- Estrogen sensitive (will enlarge during pregnancy/menstrual cycle)
- Typically occurs in 15-35 y/o women
- Biopsy: fibrous and glandular tissue
Mnemonic
fibROadenoma = estROgen sensitive
Phyllodes tumor
- Refers to a fibroepithelial tumor that ranges from benign (mostly) to malignant (rarely)
- Characteristic leaf-like projections into epithelium-lined stroma & dilated lumen
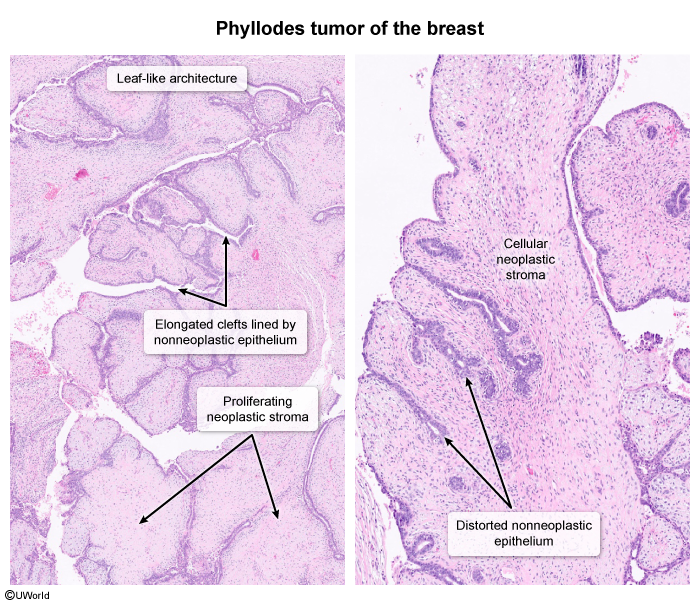
- Typically occurs in 40-50 y/o women
| Feature | Fibroadenoma | Phyllodes Tumor |
|---|---|---|
| Typical Age | Younger (15-35 yrs) | Older (40-50 yrs) |
| Prevalence | Very common, most common benign breast tumor | Rare, <1% |
| Growth | Slow, often hormone-sensitive | Can be rapid |
| Size | Usually <3 cm | Often larger |
| Histology | Benign stroma & epithelium, well-circumscribed | Increased STROMAL CELLULARITY, atypia, mitoses define grade (Benign, Borderline, Malignant). LEAF-LIKE projections. |
| Behavior | Benign | Can be benign, borderline, or malignant (hematogenous spread) |
| Recurrence | Rare after excision | Higher risk, especially if margins inadequate or higher grade |
| Management | Observation or simple excision | WIDE LOCAL EXCISION (with clear margins) is crucial for all types. |
Malignant cancer
Noninvasive carcinomas
Ductal carcinoma in situ (DCIS)
- Characteristics
- No penetration of the basement membrane
- Preceded by ductal atypia
- Frequently appears as a pattern of grouped microcalcifications on mammography
- Abnormal cell growth and death will leave calcium deposits
- Because DCIS often doesn’t cause noticeable symptoms like a lump, these microcalcifications serve as an important visual indicator.
- Higher risk of subsequent ipsilateral invasive carcinoma
- Comedocarcinoma
- Characteristics: subtype of DCIS characterized by central necrosis
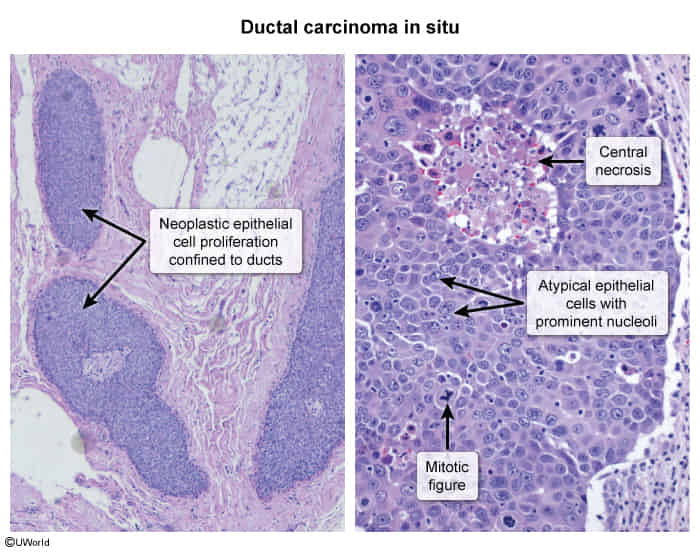
- Characteristics: subtype of DCIS characterized by central necrosis
Tip
Noninvasive carcinomas are characterized by the absence of stromal invasion.
Lobular carcinoma in situ (LCIS)
- Refers to proliferation of lobular cells but has not yet invaded basement membrane
- Lacks E-Cadherin
Mnemonic
Lobular Carcinoma Lacks Cadherin
Invasive carcinomas
Invasive ductal carcinoma (IDC)
- Characteristics
- Most common type of invasive breast cancer (∼ 80%)
- Aggressive formation of metastases
- Localization
- Unilateral
- Mostly unifocal
Medullary breast cancer
- Characteristics
- Rare subtype of invasive ductal carcinoma
- Most common tumor associated with the BRCA1 mutation
- Well-circumscribed soft tumor with smooth borders (may appear benign)
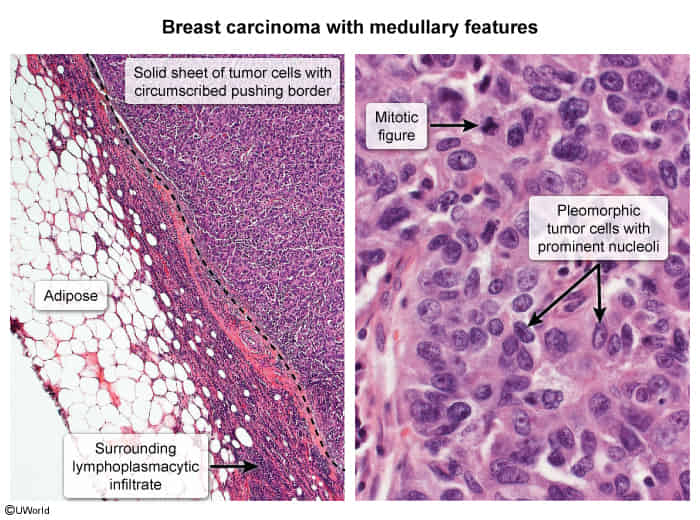
- Usually triple-negative
- Lymphadenopathy
- Differential diagnosis: fibroadenoma
Invasive lobular carcinoma (ILC)
- Characteristics
- ∼ 10% of all invasive breast carcinomas
- Less aggressive than ductal carcinoma
- Monomorphic cells in a single file pattern due to a decrease in E-cadherin expression
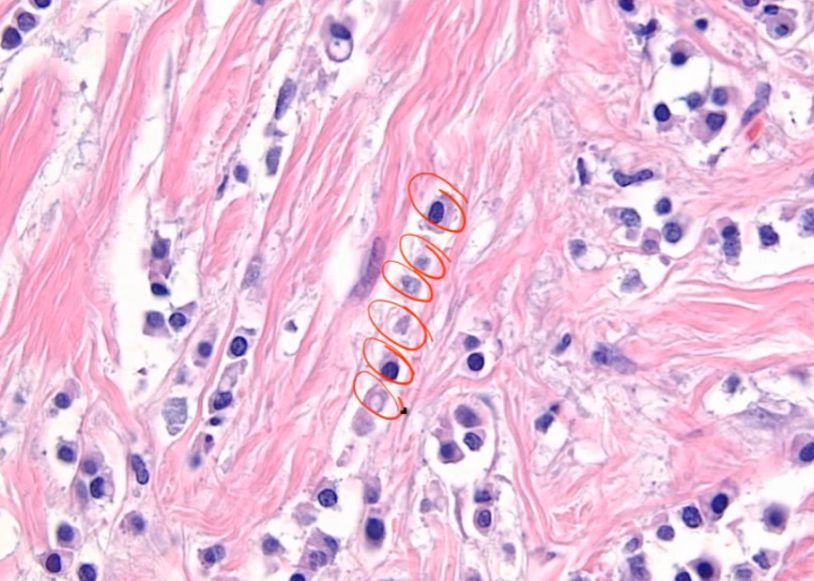
- Localization
- Bilateral in ∼ 20% of cases
- Frequently multifocal
Mnemonic
ILC = Individual Line Carcinoma
Clinical features
Locally advanced disease
- Skin
- Retractions or dimpling (due to fixation to the pectoral muscles, deep fascia, Cooper ligaments, and/or overlying skin)
- Peau d’orange (see below)
Subtypes and variants
Inflammatory conditions (DDx)
Paget disease of the breast
- Definition: a rare type of breast cancer that affects the lactiferous ducts and the skin of the nipple and areola
- Pathogenesis: migratory/epidermotropic theory: neoplastic ductal epithelial cells from an underlying DCIS or IDC move through the lactiferous ducts and invade the surrounding epidermis of the nipple.
- Clinical features

- Erythematous, scaly, or vesicular rash affecting the nipple and areola
- Pruritus; burning sensation
- Nipple retraction
- Ulceration that causes blood-tinged nipple discharge
- Diagnostics
- Punch/wedge or surface biopsy of nipple tissue: Paget cells confirm disease.
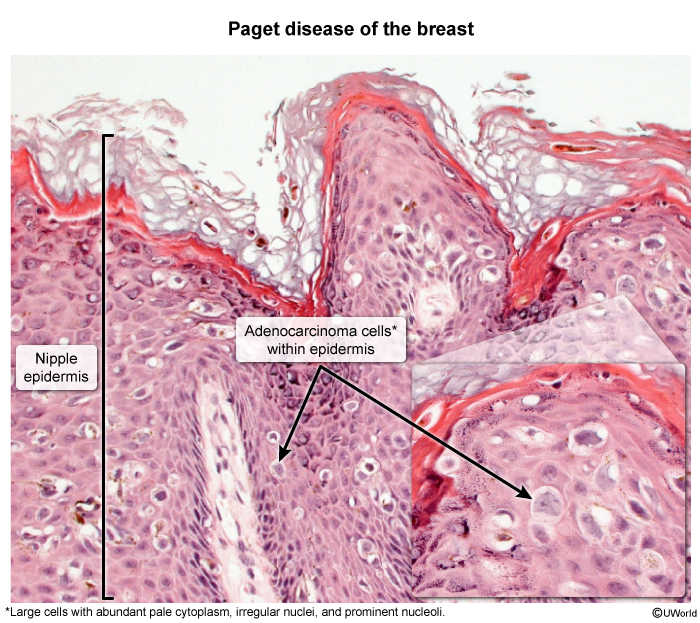
- Punch/wedge or surface biopsy of nipple tissue: Paget cells confirm disease.
Inflammatory breast cancer (IBC)
- Definition: a rare form of advanced, aggressive invasive carcinoma characterized by dermal lymphatic invasion of tumor cells
- Clinical features

- Peau d’orange
- Erythematous, warm, and edematous skin plaques with prominent hair follicles that resemble orange peel
- Caused by obstruction of the lymphatic channels due to tumor growth
- Tenderness, burning sensation
- Blood-tinged nipple discharge
- Signs of metastatic disease (e.g., axillary lymphadenopathy)
- Usually no palpable mass
- Peau d’orange
- Differential diagnosis
- Mastitis
- Fever
- No Peau d’orange
- Good response to antibiotics
- Paget disease of the breast
- Breast abscess
- Mastitis
Tip
It is called inflammatory breast cancer because its appearance resembles inflammation, but there is actually no inflammation!
Diagnostics
Receptor testing
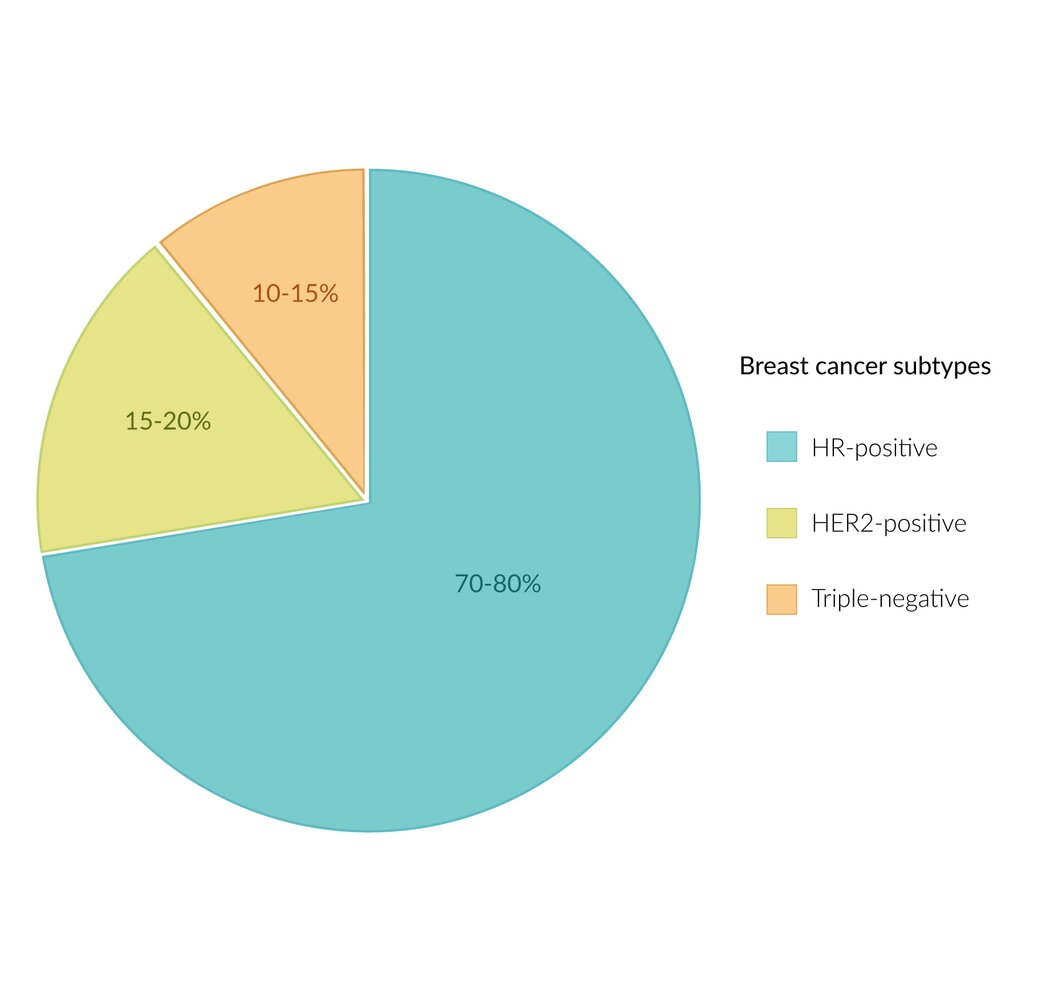
- Hormone receptors (HR) positive
- Estrogen receptor
- Progestogen receptor
- Human epidermal growth factor receptor 2 (HER2/neu, c-erbB2) positive
- Triple negative
- Ranking
- Aggressive: TN > HER2+ > HR+
- Prognosis: HR+/HER2- > HR+/HER2+ > HR-/HER2+ > TN
Treatment
Systemic therapy
ERBB2-targeted therapy (ERBB2 = HER2)
ERBB2-targeted therapy includes ERBB2 antibodies (e.g., trastuzumab, pertuzumab) and tyrosine kinase inhibitors (e.g., lapatinib, neratinib).
- Indication: all ERBB2+ tumors
- First-line agent: trastuzumab
- A humanized monoclonal antibody against the ERBB2 tyrosine kinase receptor; used in the treatment of ERBB2+ breast and gastric cancer
- Mechanism of action: targets c-erbB2 tyrosine kinase receptor → ↓ of ERBB2-initiated cellular signaling and ↑ antibody-dependent cytotoxicity → ↓ tumor growth
- Adverse effects: cardiotoxicity (e.g., dilated cardiomyopathy with systolic CHF)