Epidemiology
- Age of onset: adults > 60 years
Etiology
- The primary (idiopathic) form is most common, with age as a major risk factor.
- Secondary forms
- Joint trauma/damage: including joint surgery, previous juvenile idiopathic arthritis, and Osteoarthritis
- Metabolic disorders: including hyperparathyroidism, hemochromatosis, hypomagnesemia, hypophosphatasia, and possibly gout
- Familial chondrocalcinosis: due to mutations in the CCAL1 or CCAL2 genes
Pathophysiology
Deposition of calcium pyrophosphate dihydrate (CPP or CPPD) crystals in articular cartilage → paroxysmal joint inflammation and cartilage destruction → inflammatory arthritis (crystalline arthritis)
Clinical features
Acute CPP crystal arthritis (pseudogout)
- Clinical features
- Acute attack of pain and swelling in the affected joint(s)
- Monoarthritis (occasionally oligoarthritis)
- Most commonly affects the knee and wrist; can also affect other large joints (e.g., hips, ankles)
- Typically self-limited
- Features that differ from acute gout
- Longer duration of acute attacks
- Up to several months
- Possible systemic symptoms
- E.g., fever, chills, altered mental status in the elderly
- Longer duration of acute attacks
Chronic CPP crystal arthritis
- Osteoarthritis-like presentation (osteoarthritis with CPPD; pseudo-osteoarthritis)
Diagnostics
Arthrocentesis and synovial fluid analysis (SFA)
- Cloudy fluid
- Polarized light microscopy (with a red filter) appearance of CPP crystals (opposite to findings in Gout)
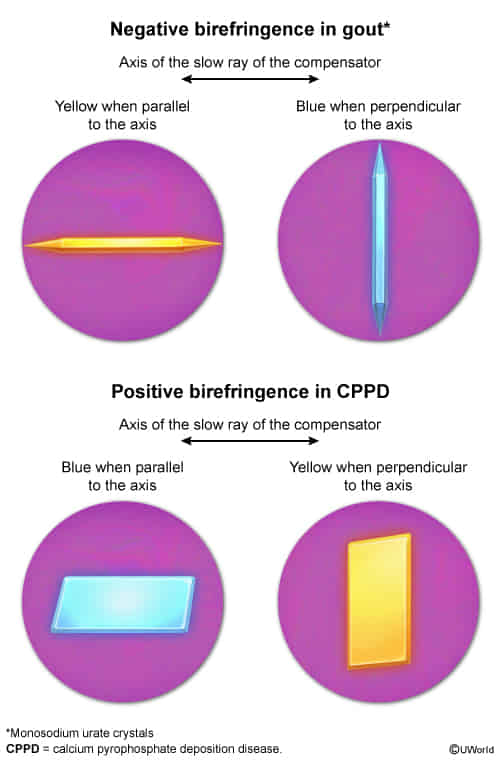
- Rhomboid-shaped crystals that are weakly positively birefringent
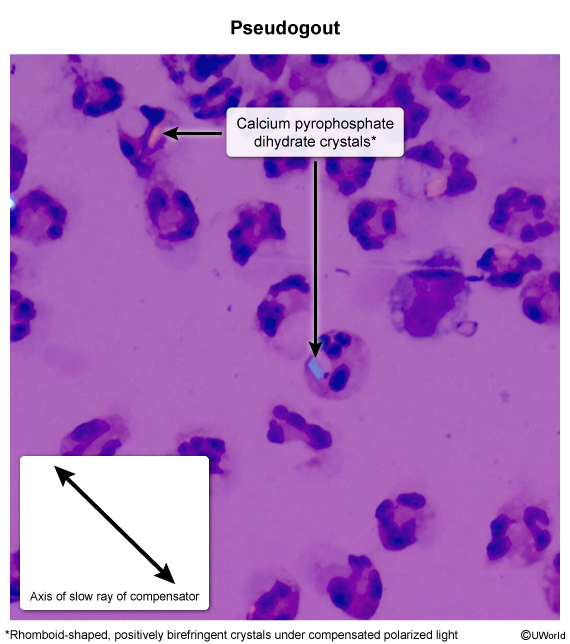
- Crystals appear blue when their optical axis is oriented parallel to the polarizer.
- Crystals appear yellow when their axis is perpendicular to the polarizer.
- Rhomboid-shaped crystals that are weakly positively birefringent
- Cell count: WBC > 2000/μL with > 50% neutrophils
Imaging
- X-ray of the affected joint(s)
- Chondrocalcinosis: calcification of cartilage in the affected joints

- Chondrocalcinosis: calcification of cartilage in the affected joints