Epidemiology
- Most common cause of hyperthyroidism in the United States
Etiology
- Genetic predisposition
- 50% of patients with Graves disease have a family history of autoimmune disorders (e.g., type 1 diabetes mellitus, Hashimoto disease, pernicious anemia, myasthenia gravis)
- Associated with HLA-DR3 and HLA-B8 alleles
- Autoimmunity: B and T lymphocyte-mediated disorder
- Triggers
- Infectious agents: Yersinia enterocolitica and Borrelia burgdorferi have been shown to trigger antigen mimicry for homologies between their protein constituents and thyroid autoantigens.
- Stress
- Stress causes cortisol-mediated immune suppression, which is often followed by rebound immunologic hyperactivity and can trigger Graves disease in genetically susceptible individuals.
- Physical: surgery, trauma
- Psychological
- Pregnancy
- Thyroid overstimulation by high levels of hCG and TRAb during the first trimester increases the risk of Graves disease in the first trimester of pregnancy. In the second trimester, the risk decreases due to progesterone-induced immunosuppression. The risk of Graves disease increases postpartum in susceptible patients due to a drop in progesterone level which leads to the rebound of the immune system that can trigger autoimmunity.
Pathophysiology
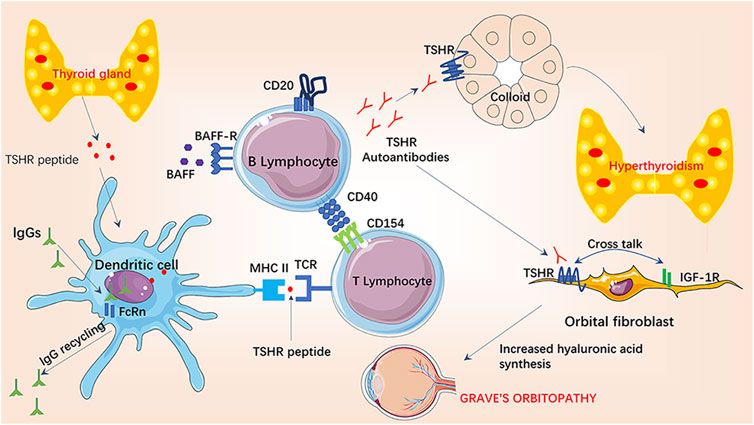
- General mechanism: B and T cell-mediated autoimmunity → production of stimulating immunoglobulin G (IgG) against TSH-receptor (TRAb; type II hypersensitivity reaction) → ↑ thyroid function and growth → hyperthyroidism and diffuse goiter
- Thyroid-associated ophthalmopathy
- TSH receptor is also present on fibroblasts in eyes
- Activated B and T cells infiltrate retro-orbital space targeting orbital fibroblasts → cytokine release (e.g. TNF-α, IFN-γ) → local inflammatory response → stimulates fibroblasts to secrete glycosaminoglycans (hyaluronic acid), which also pulls water into the interstitial space (osmotic effect) → expansion of retro-orbital tissue due to increased fluid in extraocular muscles, lymphocytic infiltration, and adipogenesis
- Pretibial myxedema: dermal fibroblast stimulation and deposition of glycosaminoglycans in connective tissue
Tip
Although the majority of symptoms are due to increased thyroid hormone levels, myxedema (nonpitting edema) and exophthalmos in patients with Graves disease are instead due to autoantibody-mediated activation of TSH receptors on peripheral tissue. Therefore they are not seen on other Hyperthyroidism diseases.
Clinical features
Diagnostics
Pathology
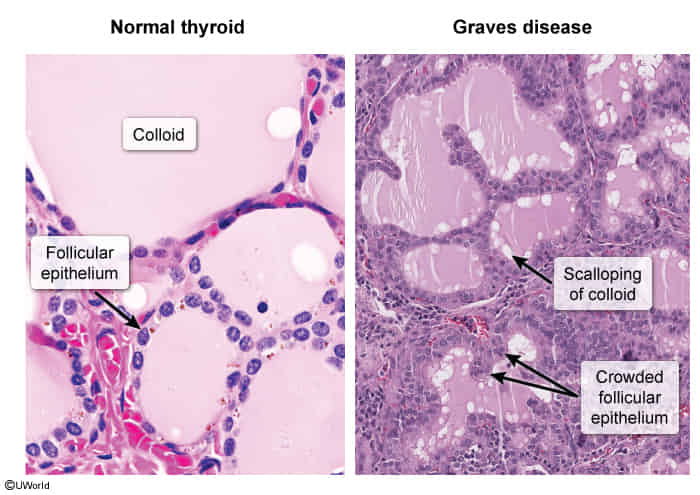
- Microscopic: histological features of an overactive gland
- Diffuse hyperplasia of thyroid follicles
- Tall, hyperplastic and hypertrophic follicular cells
- Hyperactive reabsorption causes scalloping around the edges of the colloid
Treatment
- Graves ophthalmopathy
- High-dose IV steroids
- Glucocorticoids decrease the severity of inflammation and reduce the excess extraocular volume.
- High-dose IV steroids