Epidemiology
Etiology
Embolic strokes (∼ 20% of all strokes)
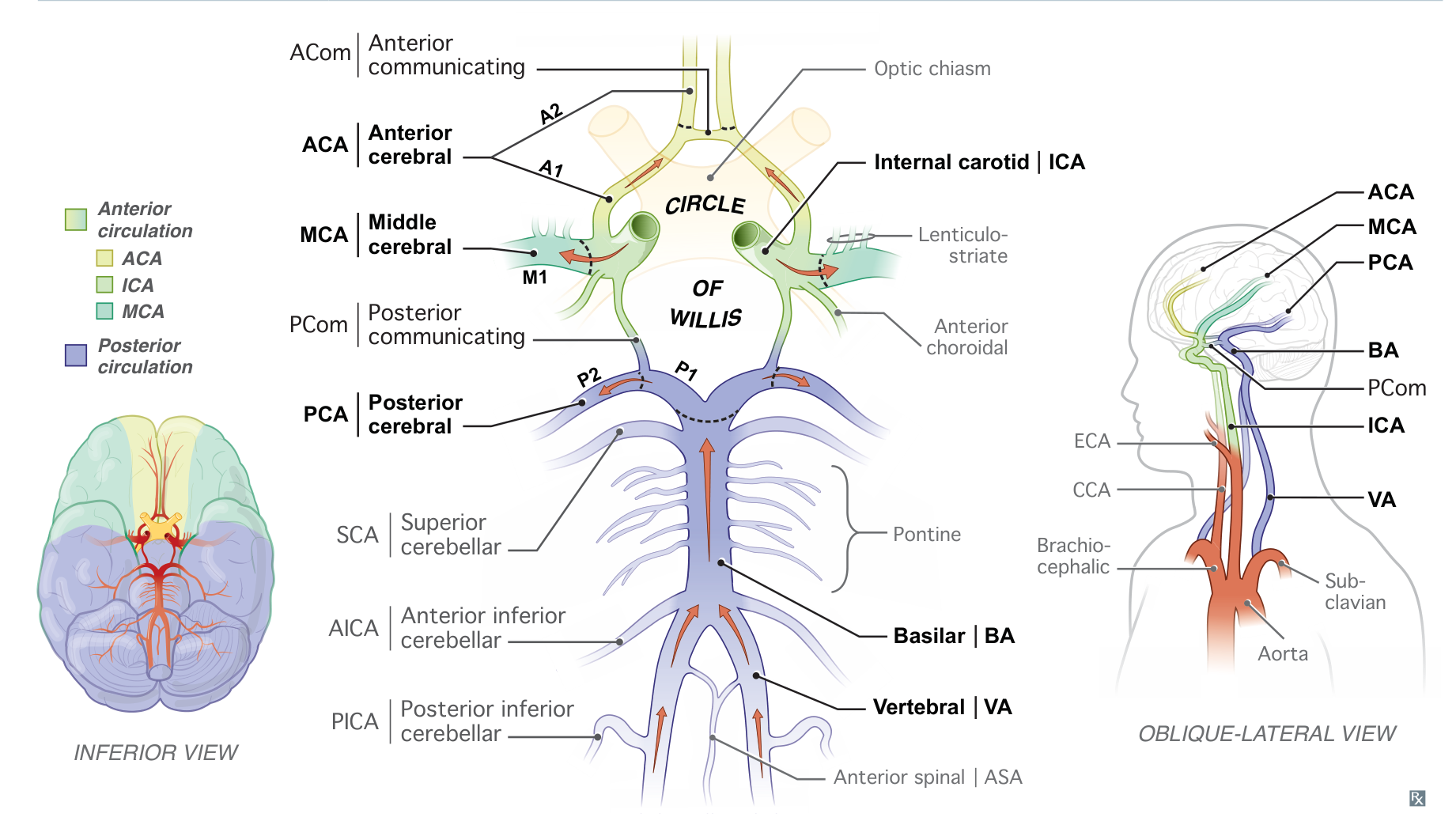
- Most commonly affect the middle cerebral artery (MCA)
- Likely cause multiple scattered infarcts in an asymmetric pattern within different major vascular territories (eg, middle and anterior cerebral artery)
Thrombotic strokes (∼ 40%)
- Large vessel atherosclerosis (∼ 20%)
- Rupture of an atherosclerotic plaque and exposure of subendothelial collagen → formation of a thrombus
- Thrombus formation most commonly occurs at branch points in arteries (e.g., internal carotid artery bifurcation or where the MCA branches from the circle of Willis).
- Small vessel occlusion (e.g., lacunar infarct) (∼ 20%)
Global cerebral ischemia
- Systemic hypoperfusion
- Shock or bilateral large artery atherosclerosis (e.g., of carotid arteries) → decreased effective oxygen delivery to the whole brain
- Common during cardiac surgeries
- Can result in watershed infarct
- Hypoglycemia: Repeated episodes of hypoglycemia (e.g., due to insulinoma) increase the risk of cerebral ischemia.
- Severe and/or chronic hypoxia: hypoxemia (e.g., due to respiratory arrest) → global tissue hypoxia in the brain
Classifications
Tip
Most vulnerable: hippocampus (CA1 region), neocortex, cerebellum (Purkinje cells), watershed areas (“vulnerable hippos need pure water”).
Anterior circulation
Posterior circulation
Posterior cerebral artery
A left posterior cerebral artery stroke can lead to alexia without agraphia in which someone is unable to read but can still write, speak, and listen.
Mnemonic
Someone cannot read letters if the post office workers have left for the day.
Anterior spinal artery
Medial medullary syndrome involves contralateral hemiplegia, contralateral epicritic numbness, and ipsilateral tongue weakness.
Mnemonic
“MM! These açaí (ASA-i) berries are so tasty I want to lick them!”
Posterior inferior cerebellar artery (Wallenberg syndrome, lateral medullary syndrome)
Lateral medullary syndrome involves loss of protopathic sensation in the contralateral extremities and ipsilateral face, ipsilateral Horner’s syndrome, cerebellar signs, dysarthria, and dysphagia.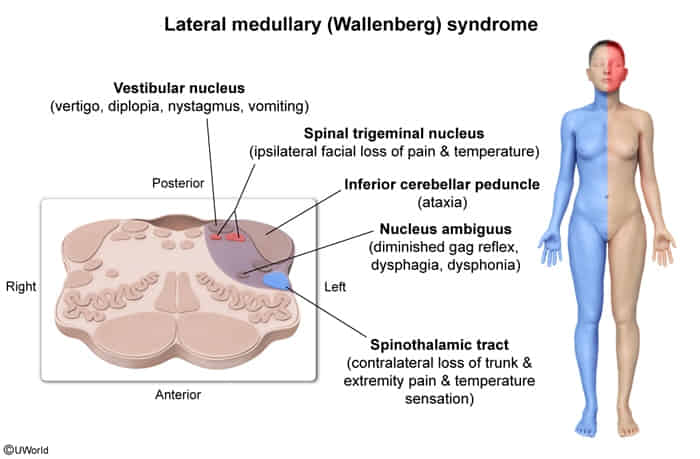
Mnemonic
PICA-chew: A Posterior Inferior Cerebellar Artery stroke makes it so you can’t chew.
Anterior inferior cerebellar artery (Lateral pontine syndrome)
Lateral pontine syndrome is similar to lateral medullary syndrome but also involves facial paralysis and hearing loss.
Mnemonic
A stroke in the Anterior Inferior Cerebellar Artery messes up the fAICAl nerve.
Basilar artery (Locked-in syndrome)
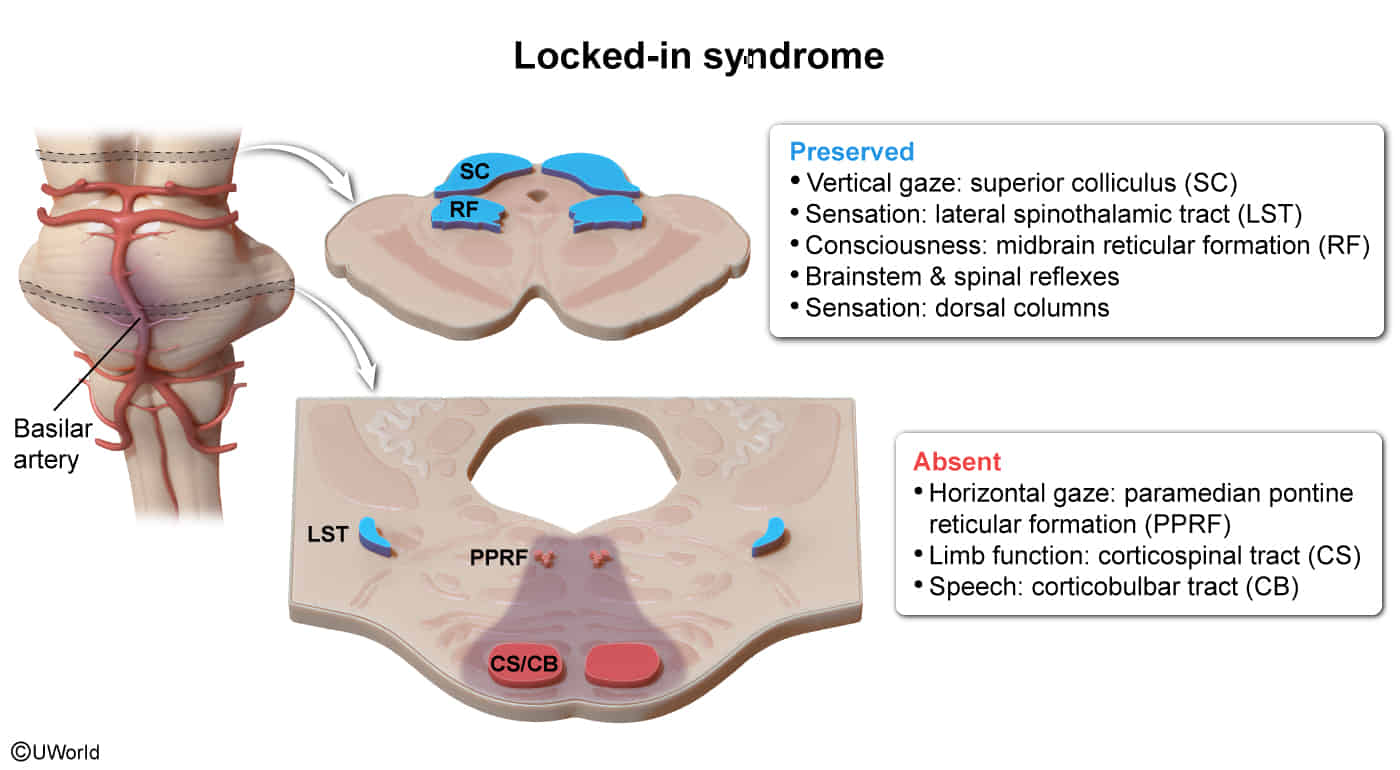
- Etiology
- Bilateral ventral pontine stroke (most common)
- Ischemic stroke (thrombotic/embolic occlusion of the basilar artery)
- Hemorrhagic stroke
- Pontine demyelination (e.g., multiple sclerosis affecting the ventral pons, central pontine myelinolysis)
- Brain tumor or brain abscess affecting the ventral pons
- Bilateral ventral pontine stroke (most common)
- Clinical features
- Caused by ischemic injury to the bilateral ventral pons
- Absent voluntary motor function of all limbs (quadriplegia) and oral structures (loss of speech) due to destruction of the cortical spinal and cortical bulbar pathways, which prevents cranial nerves or the limbs from receiving cortical signals.
- Absent horizontal eye movements. However, vertical eye movements and eyelid elevation are preserved because they are controlled in the rostral midbrain.
- Preserved consciousness because the midbrain reticular formation is spared. Behavioral arousal and sleep-wake cycles are also preserved because the diencephalon–upper brainstem arousal systems are unaffected.
- Preserved sensation because sensory pathways are not affected and preserved brainstem and spinal reflexes because they do not require cortical input.
Mnemonic
Locked-in syndrome (locked in the basement).
Pathophysiology
Clinical features
Subtypes and variants
Lacunar infarction
- Definition: noncortical infarcts characterized by the absence of cortical signs (e.g., no aphasia, hemianopsia, agnosia, apraxia)
- Etiology
- Most common: chronic hypertensive vasculopathy → lipohyalinosis of the small vessels → occlusion of small, penetrating arteries (e.g., lenticulostriate artery) → lacunar stroke resulting in specific lacunar syndromes
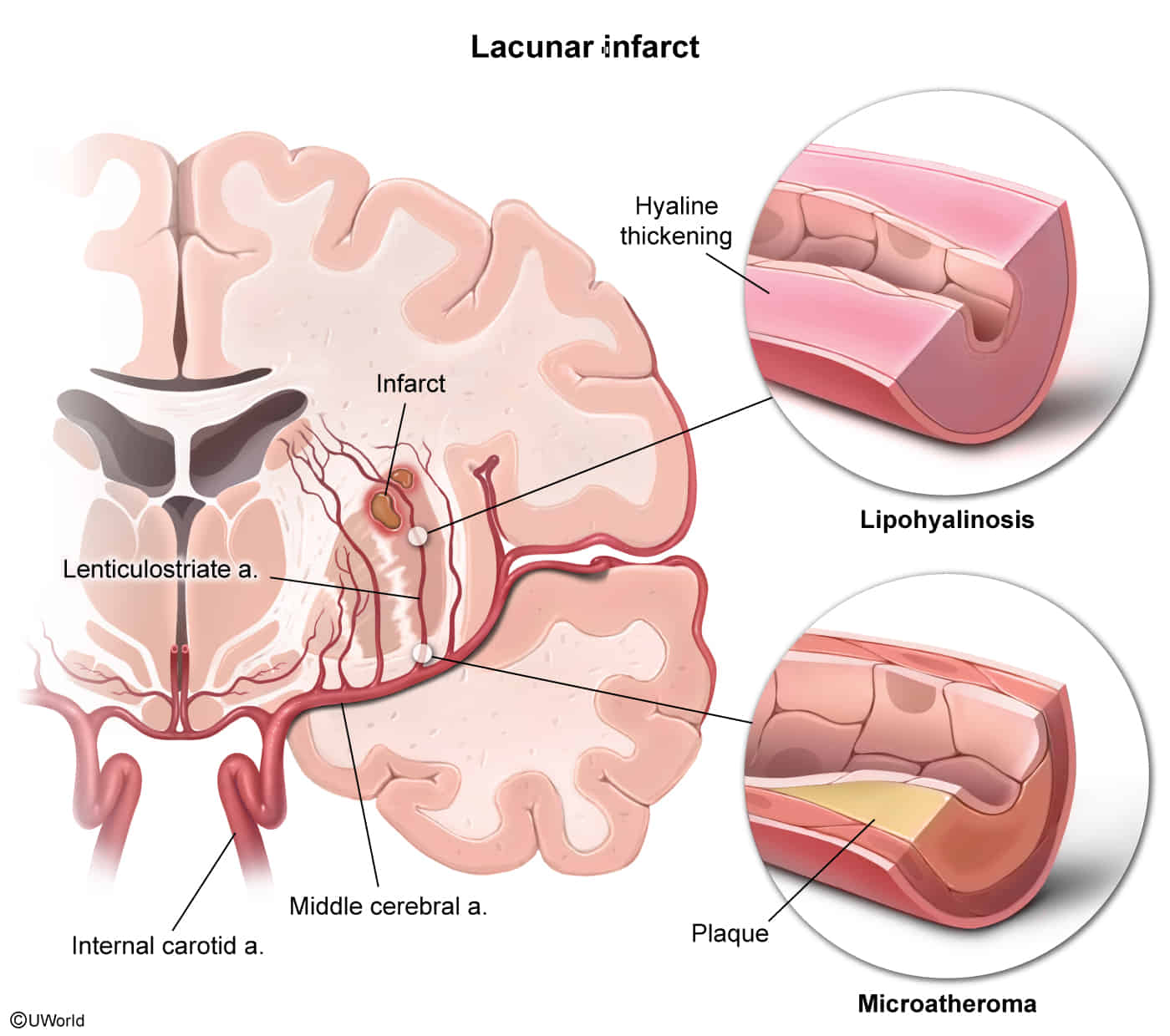
- Most common: chronic hypertensive vasculopathy → lipohyalinosis of the small vessels → occlusion of small, penetrating arteries (e.g., lenticulostriate artery) → lacunar stroke resulting in specific lacunar syndromes
- Risk factors
- Clinical features
- Pure motor stroke
- Location
- Posterior limb of the internal capsule (most common)
- May also involve striatum, corona radiata, basal pons, medial medulla
- Often caused by occlusion of the lenticulostriate artery
- Clinical features
- Contralateral hemiparesis of the face, arm, and leg (causes circumduction gait)
- No sensory impairment
- Most common type of lacunar stroke (> 50%)
- Location
- Pure motor stroke
Tip
If an infarction causes abnormalities in multiple body parts (e.g., legs + arms + face), it is unlikely to be a cortical infarction, because the cortical areas corresponding to different parts are supplied by different vessels. A thalamic (sensory) or internal capsule (motor) infarction is more likely.
Watershed infarct
- Definition: border-zone infarct in the region between the territory of two major arteries that supply the brain (watershed area)
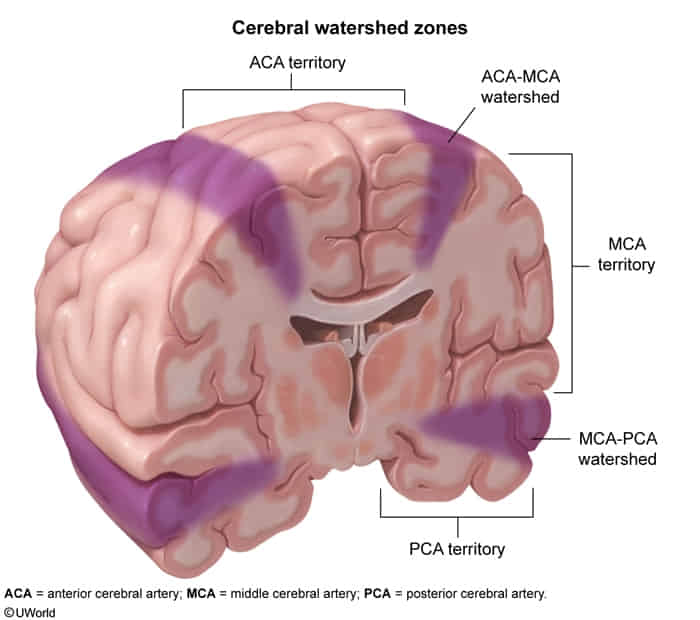
- Etiology: sudden decrease in blood pressure or cessation of blood flow through both vessels → ischemia in the susceptible region between two vascular territories
- Cortical border zones: territories between the anterior and middle cerebral arteries and between the middle and posterior cerebral arteries
- Internal border zones: territories between the superficial and deep branches of the MCA
- Clinical features
- Signs of systemic hypoperfusion (e.g., tachycardia, low blood pressure, pallor, sweating)
- Diffuse neurological deterioration
- PCA-MCA watershed region: bilateral visual loss (cortical blindness)
- ACA-MCA watershed region: proximal limb weakness with sparing of the face, hands, and feet (“man-in-the-barrel syndrome”)
Diagnostics
Pathology
- 12-24 hours
- Microscopic: Red neurons (eosinophilic cytoplasm, pyknotic nuclei, loss of Nissl substance)
- Macroscopic: No significant changes
- 24-72 hours
- Microscopic: Neutrophilic infiltration
- Macroscopic: No significant changes
- 3-7 days
- Microscopic: Macrophage/microglia infiltration & phagocytosis begins
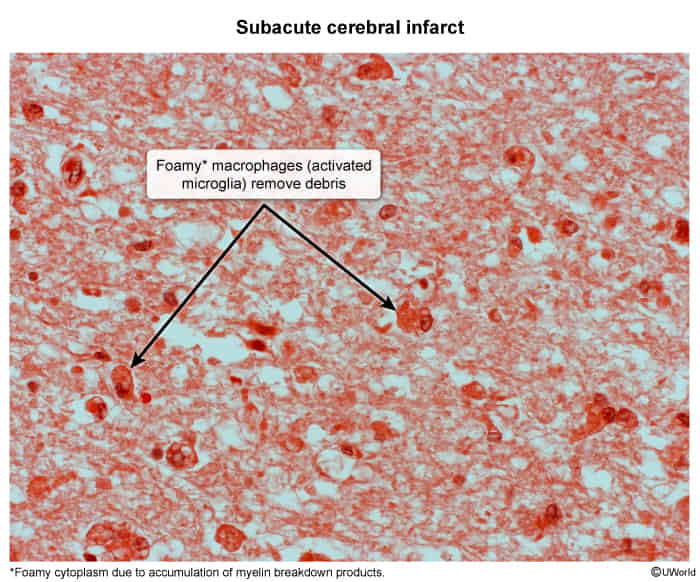
- Macroscopic: No significant changes
- Microscopic: Macrophage/microglia infiltration & phagocytosis begins
- 1-2 weeks
- Microscopic: Reactive gliosis & vascular proliferation around the necrotic area
- Macroscopic: Liquefactive necrosis (continues 1 week-1 month)
- >2 weeks
- Microscopic: Glial scar formation
- Macroscopic: Cystic area surrounded by dense glial fibers (develops after >1 month)