Epidemiology
Etiology
Inciting event
- Traumatic EDH
- Head injury (most common; e.g., due to motor vehicle accidents, falls, assault)
Source of hemorrhage
- Arterial EDH
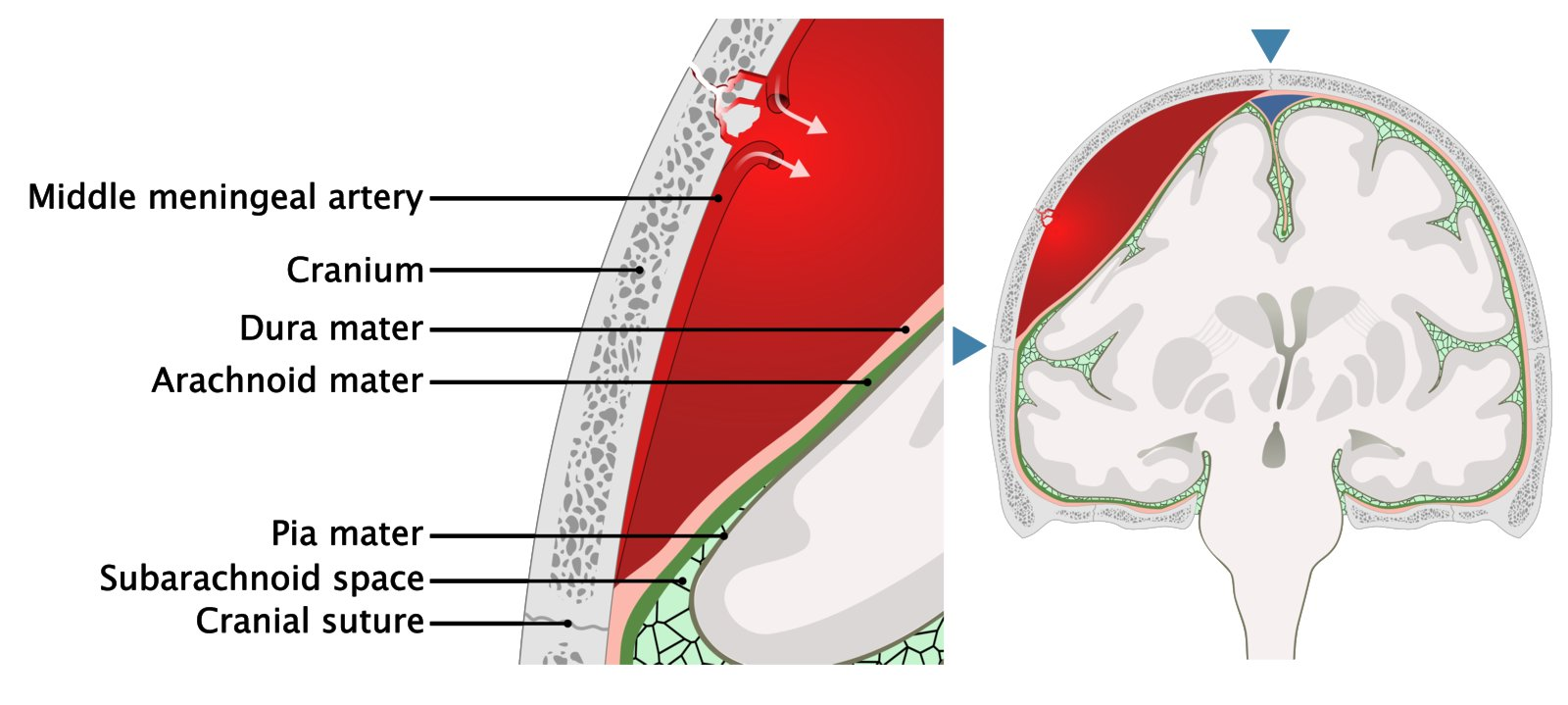
- Source: middle meningeal artery rupture or tear (a branch of the maxillary artery and the most common source of hemorrhage in EDH)
- Sites of rupture
- Pterion (most common): the thinnest part of the skull and a site at which the middle meningeal artery lies in close proximity to the skull
Pathophysiology
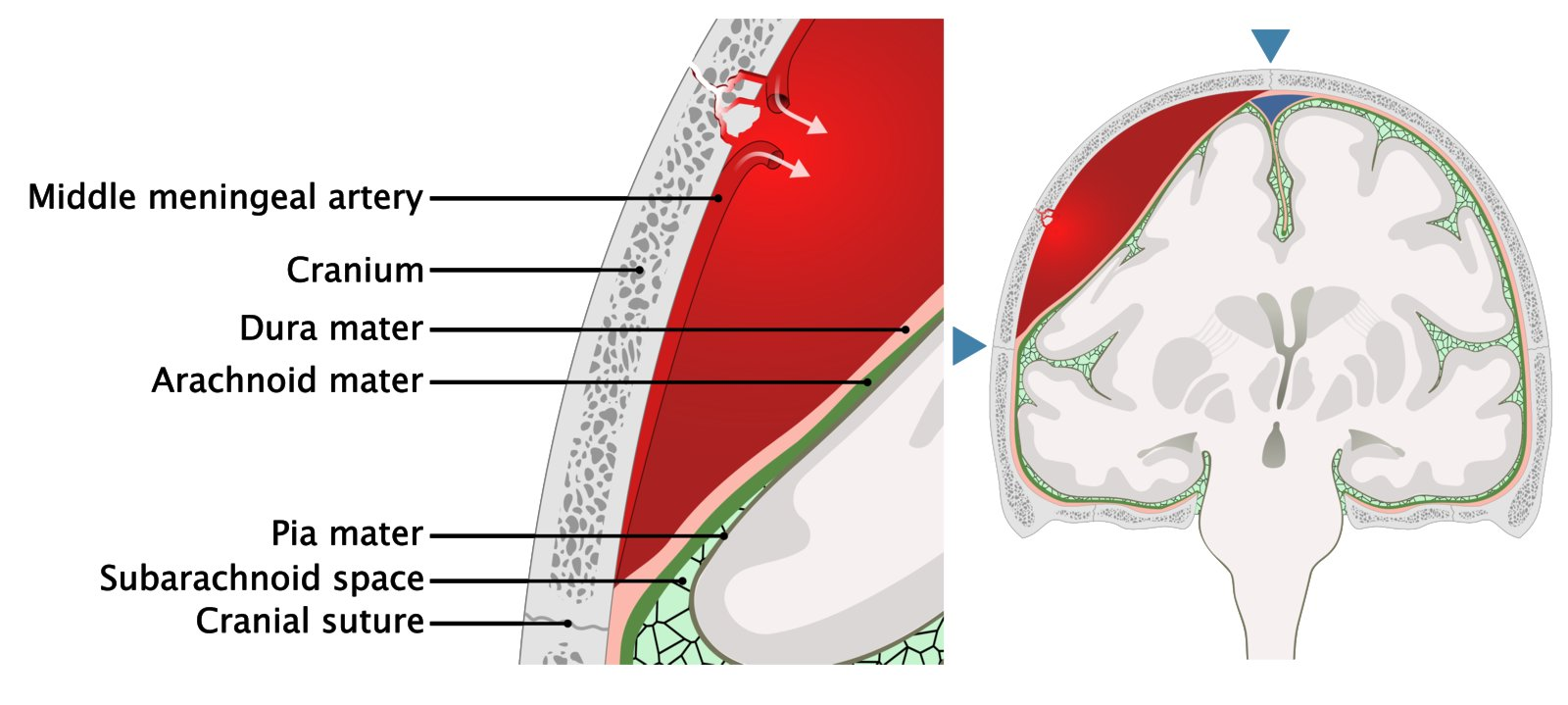
- Venous shunting of blood out from the epidural space and initial asymptomatic compression of the anterior temporal lobe → lucid interval
- Continued expansion of EDH → increased intracranial pressure → transtentorial uncal herniation (Monro-Kellie principle) which leads to:
- Compression of the ipsilateral oculomotor nerve and loss of parasympathetic supply to the pupillary sphincter → ipsilateral dilated pupil (anisocoria)
- Compression of the brain stem → rapid neurological decline, Cushing triad
Clinical features
- Classic presentation of EDH
- Initial loss of consciousness immediately following a head injury
- Temporary recovery of consciousness with return to normal or near-normal neurological function (lucid interval)
- Renewed decline in neurological status and onset of symptoms caused by hematoma expansion and mass effect:
- Contralateral focal neurological deficits
- Signs of ↑ ICP (e.g., headache, Cushing triad)
- Pupillary abnormalities (sign of uncal herniation)
- Anisocoria with ipsilateral mydriasis (most common)
- Unilateral or bilateral fixed dilated pupils
- Potentially contralateral or bilateral mydriasis
- Signs of cerebral herniation syndromes
Diagnostics
Differential diagnostics
See Intracranial hemorrhage
Treatment