Epidemiology
- AMD is the leading cause of blindness in individuals > 65 years in developed countries.
- Age of onset: usually > 55 years
Etiology
- Risk factors
- Advanced age
- Cardiovascular disease
- Smoking
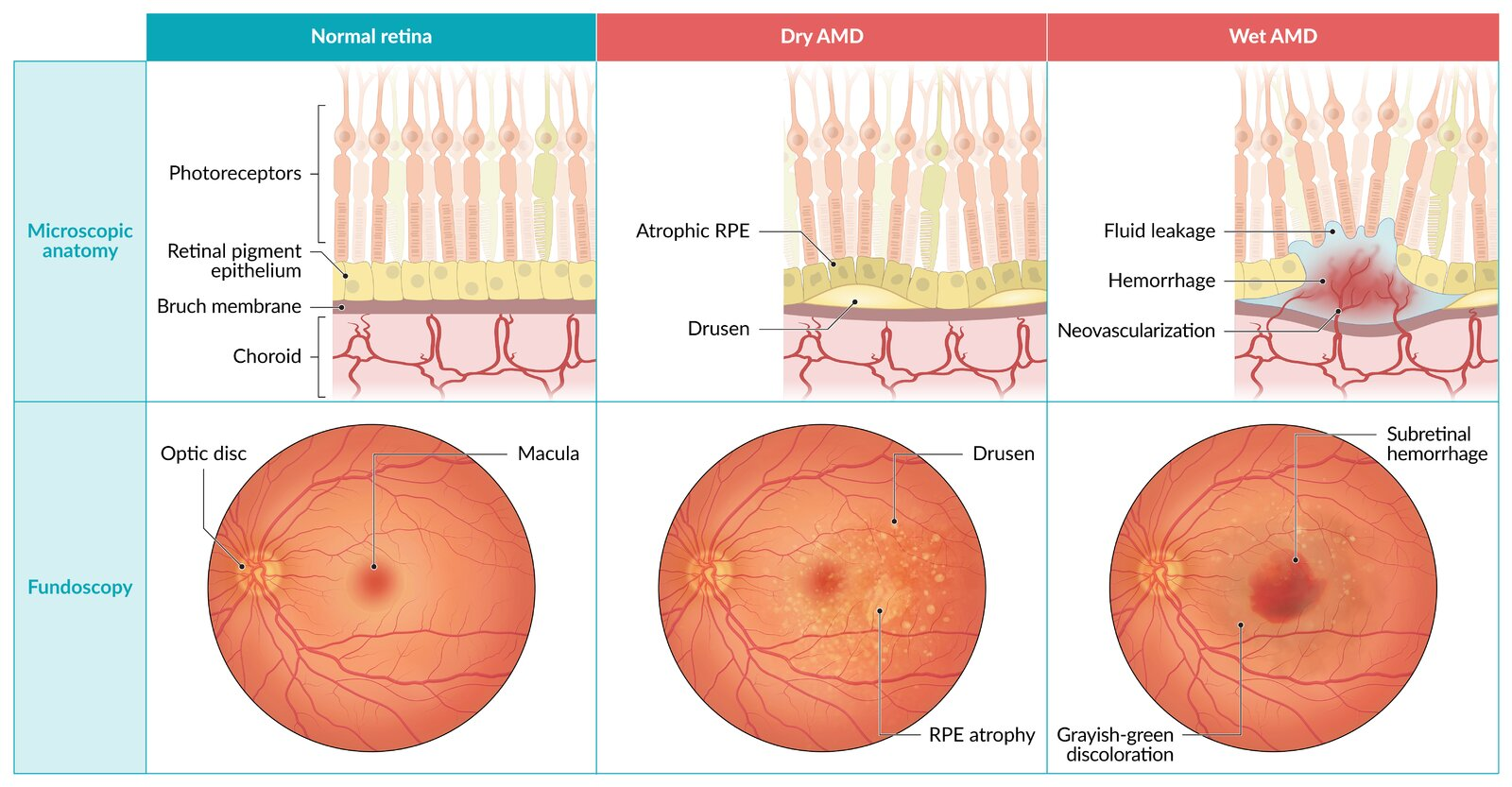
Pathophysiology
AMD is characterized by progressive degenerative changes in the central part of the retina (macula) → visual impairment.
- Dry AMD (∼ 90%)
- Also referred to as nonexudative AMD or atrophic AMD
- Deposition of yellow-whitish material consisting of lipids, vitronectin, and other proteins (drusen) in the retinal pigment epithelium and between it and Bruch membrane → slow progressive atrophy of the local retinal pigment epithelium (centrally or pericentrally)
- The condition likely results from chronic oxidative damage to the retinal pigment epithelium and choriocapillaris, leading to subretinal inflammation with abnormal extracellular matrix formation (eg, confluent drusen, basement membrane thickening).
- Wet AMD (∼ 10%)
- Also referred to as exudative AMD or neovascular AMD
- Choroidal neovascularization (between the retinal pigment epithelium and Bruch’s membrane) → leaking of intravascular serous fluid and blood → sudden localized elevation of the macula and/or detachment of the retinal pigment epithelium
- Hemorrhages can cause sudden loss of vision.
Clinical features
- Painless central or pericentral visual impairment → reduced visual acuity, difficulty adapting to changes in lighting
- Dry AMD: slow progressive visual impairment (usually over decades) and unilateral or bilateral onset
- Wet AMD: acute or insidious onset (over weeks to months) and usually manifests in one eye first
- Metamorphopsia: type of visual distortion in which straight lines appear wavy, which can be tested for using an Amsler grid
- Scotoma (blind spot)
Diagnostics
- Amsler grid: detection of metamorphopsias and scotomas
- Fundoscopy
- Dry AMD
- Drusen
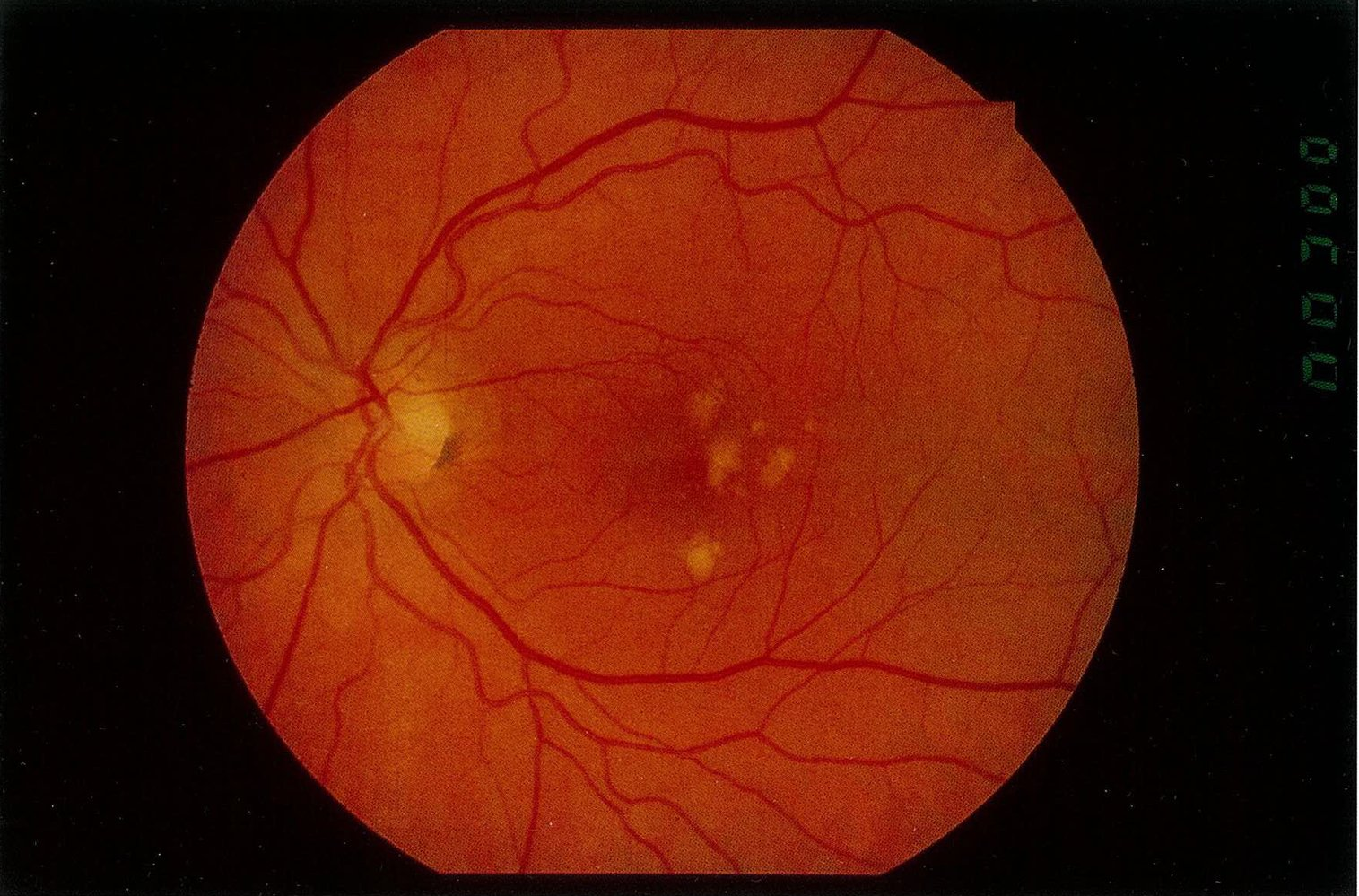
- Drusen
- Wet AMD
- Subretinal and intraretinal hemorrhage and/or exudate
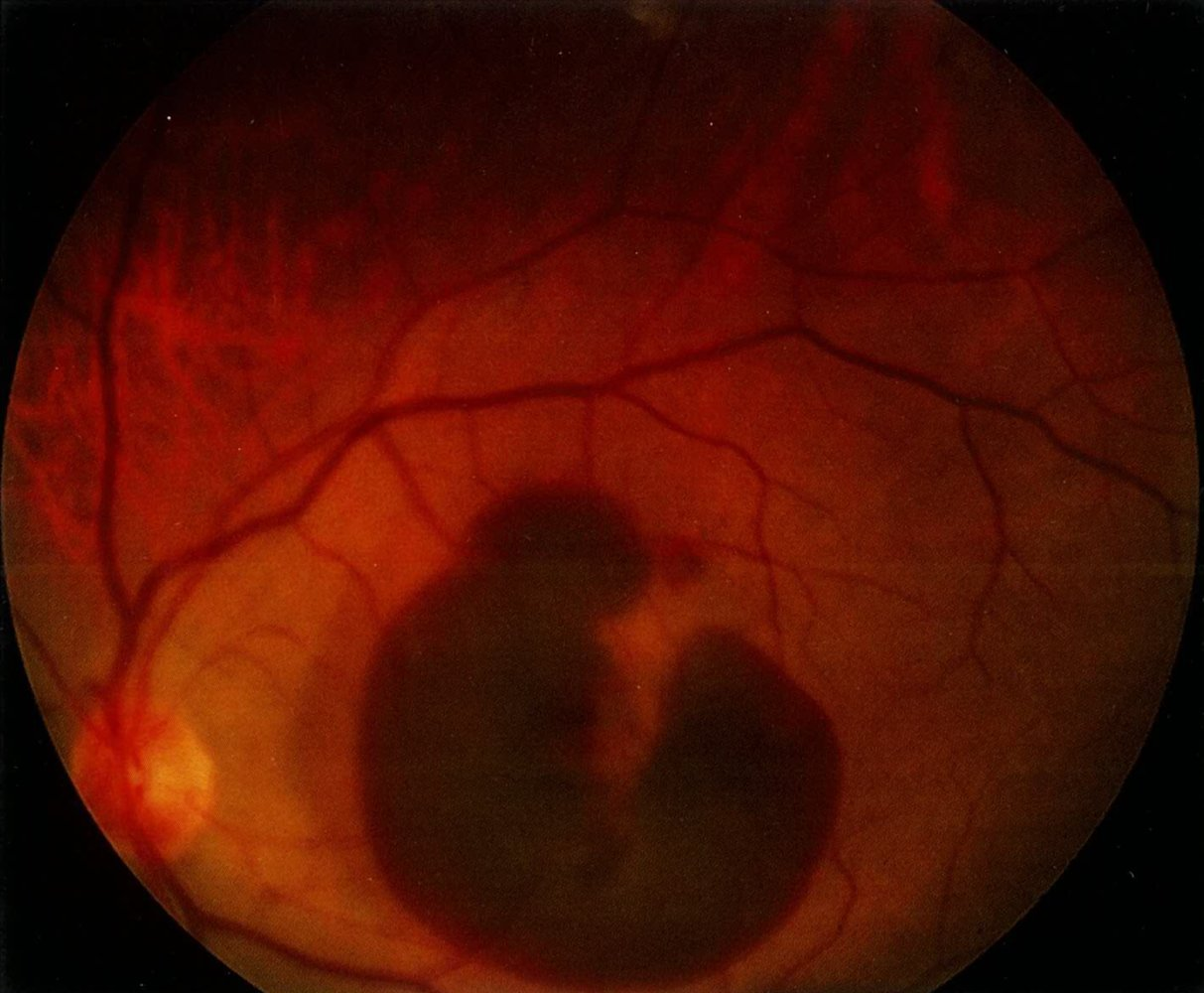
- Subretinal and intraretinal hemorrhage and/or exudate
- Dry AMD
Treatment
- Treatment of wet AMD
- First-line: injection of VEGF inhibitors (ranibizumab, bevacizumab, pegaptanib) into the vitreous body
Mnemonic
Ranibizumab → bizu 两个眼珠