Etiology
Pathophysiology
COPD is characterized by chronic airway inflammation and tissue destruction.
Chronic airway inflammation
It results from significant exposure to noxious stimuli, increased oxidative stress (most commonly due to cigarette smoke) as well as by increased release of reactive oxygen species by inflammatory cells.
- Increased number of neutrophils, macrophages, and CD8+ T lymphocytes → release of cytokines → amplification of inflammation and induction of structural changes of lung parenchyma (e.g., via stimulation of growth factor release)
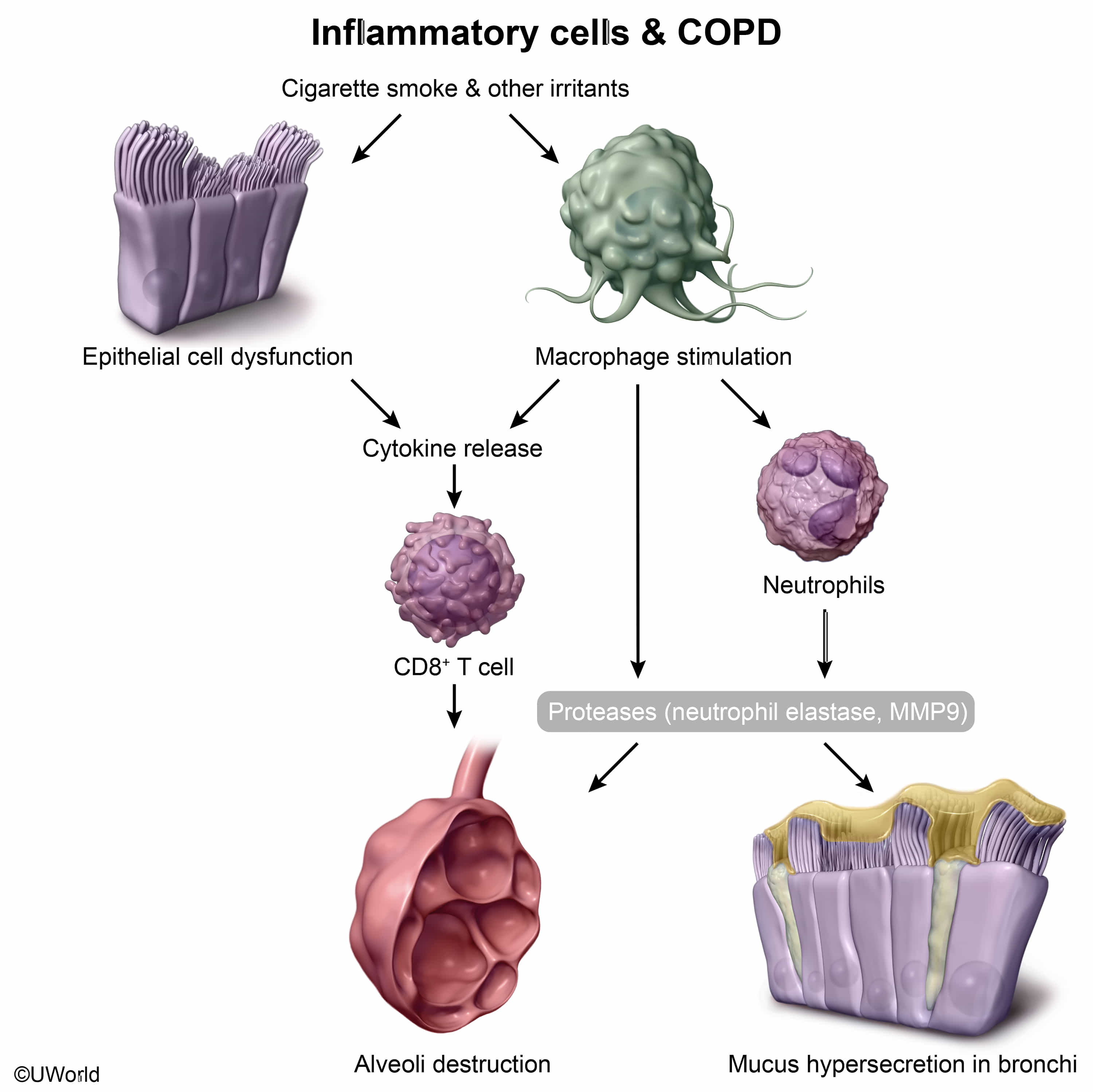
- CD8+ T lymphocytes mediate inflammation in individuals with COPD.
- CD4+ T lymphocytes and eosinophils mediate inflammation in individuals with bronchial asthma.
- Promotion of goblet cell proliferation and hypertrophy, mucus hypersecretion, and impaired ciliary function → chronic productive cough
- Reid index is the ratio of the thickness of the submucosal mucus-secreting glands to the thickness between the epithelium and cartilage in the bronchial tree.

- Reid index > 0.5 is characteristic of chronic bronchitis.
- Reid index is the ratio of the thickness of the submucosal mucus-secreting glands to the thickness between the epithelium and cartilage in the bronchial tree.
- Smooth muscle hyperplasia of the small airways and pulmonary vasculature (mainly due to hypoxic vasoconstriction) → pulmonary hypertension → cor pulmonale
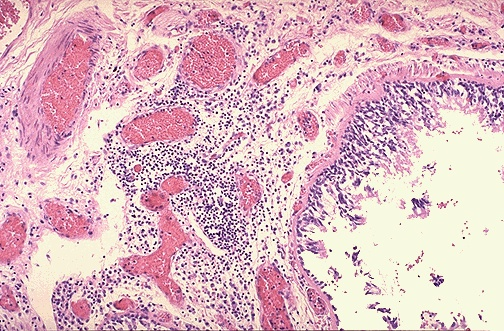
This photomicrograph shows a bronchus with increased numbers of chronic inflammatory cells in the submucosa. Chronic bronchitis does not have characteristic pathologic findings, but is defined clinically as a persistent productive cough for at least three consecutive months in at least two consecutive years. Most patients are smokers. Often, there are features of emphysema as well. Since chronic bronchitis and emphysema often overlap, the term ‘chronic obstructive pulmonary disease’ (COPD) can be applied.
Tissue destruction
- Bronchopulmonary inflammation → ↑ proteases
- Nicotine use (or other noxious stimuli) inactivates protease inhibitors (especially α1-antitrypsin) → imbalance of protease and antiprotease → ↑ elastase activity → loss of elastic tissue and lung parenchyma
Subtypes and variants
Emphysema subtypes
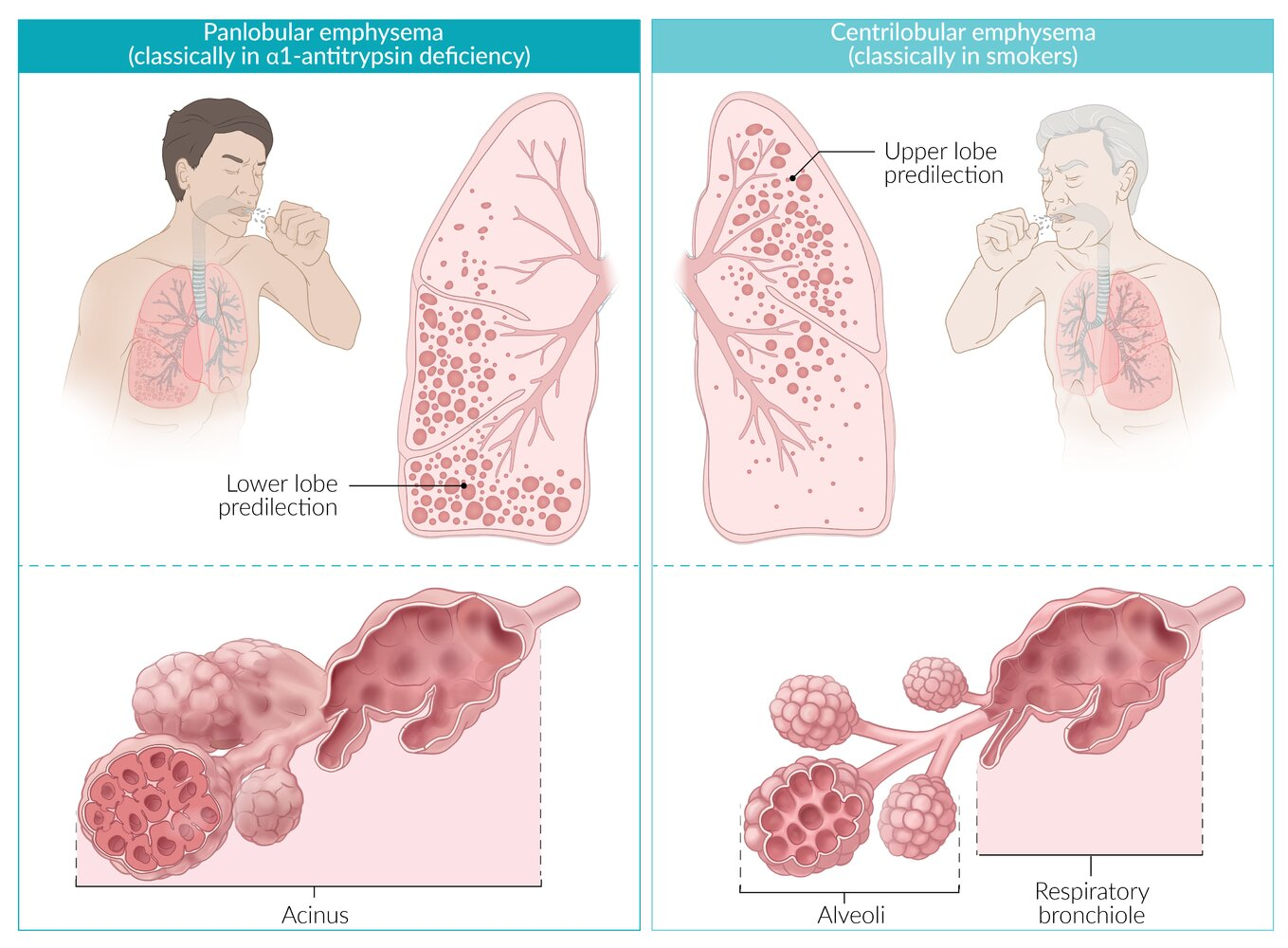
- Centrilobular emphysema (centriacinar emphysema)
- Most common type of emphysema
- Classically seen in smokers
- Characterized by the destruction of the respiratory bronchiole (central portion of the acinus); spares distal alveoli
- Usually affects the upper lobes
- Panlobular emphysema (panacinar emphysema)
- Rare type of emphysema
- Associated with AATD
- Characterized by the destruction of the entire acinus (respiratory bronchiole and alveoli)
- Usually affects the lower lobes
- Tobacco exposure dramatically accelerates the development of emphysema in patients with AAT deficiency by inducing inflammation (increasing neutrophil and macrophage activation) and permanently oxidizing and inactivating AAT. Therefore, patients with AAT deficiency should be counseled to avoid smoking and exposure to second-hand smoke.
Mnemonic
“Smoke rises up:” Centriacinar emphysema is associated with smoking and primarily involves the upper lobes of the lungs.
Clinical features
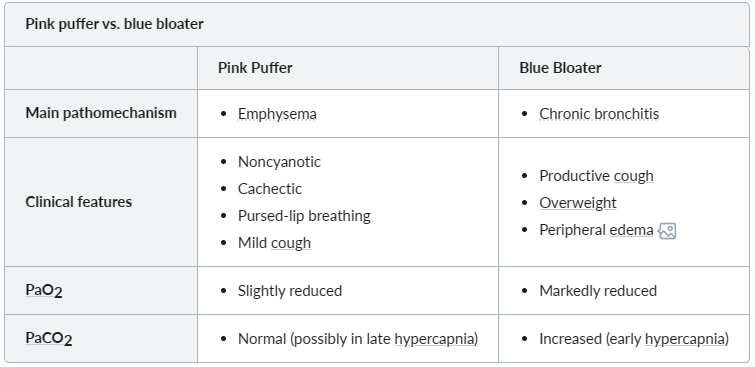
Pink puffer and blue bloater
Diagnostics
Mnemonic
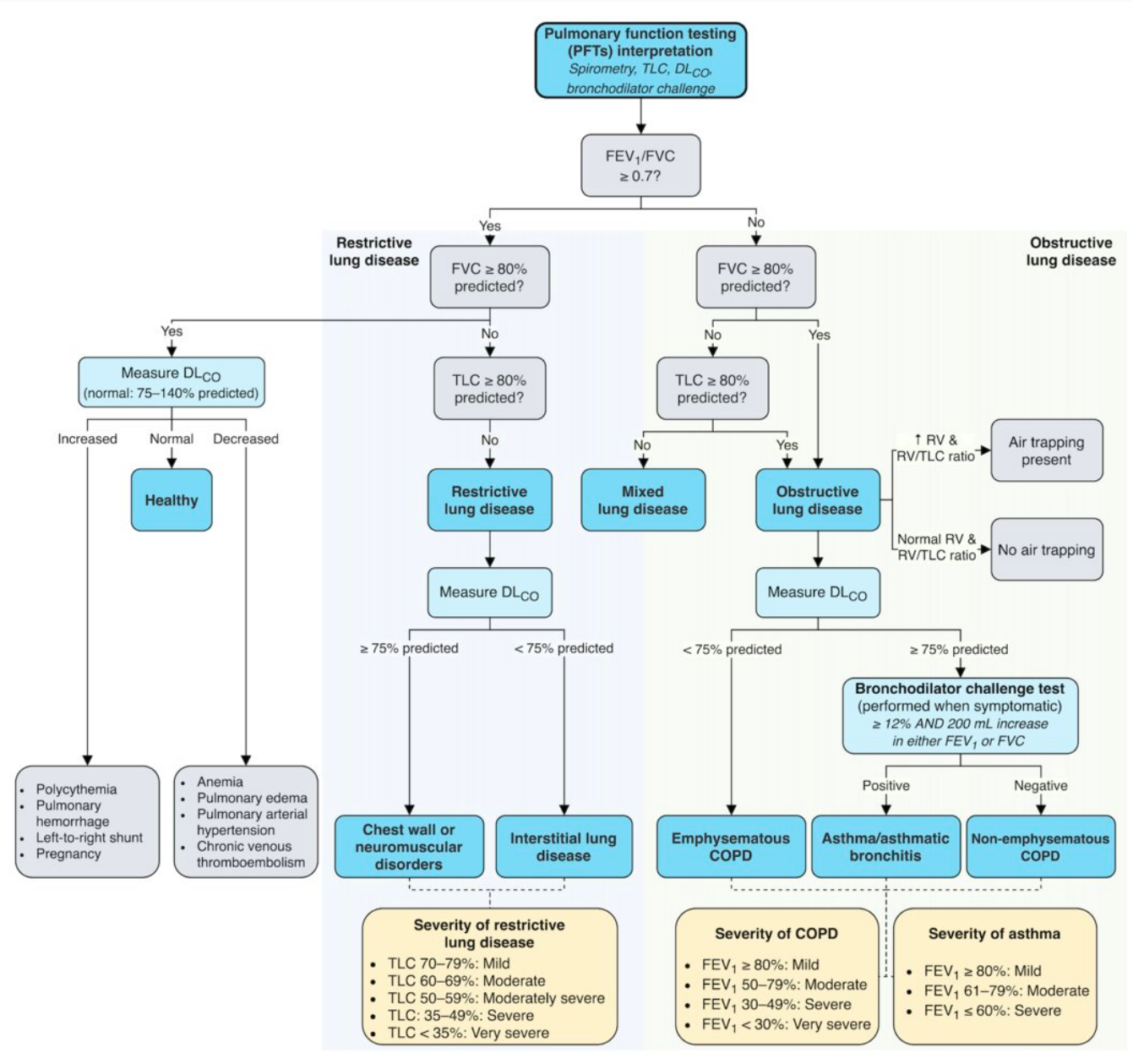
FEV1/FVC ratio: Obstructive: Obscures the ratio Restrictive: Raises the ratio (or at least Remains constant)
Treatment
Acute exacerbation of COPD (AECOPD)
AECOPD is a clinical diagnosis based on the development of cardinal symptoms of AECOPD (e.g., acute worsening dyspnea, increase in the purulence of sputum) over ≤ 14 days. It is often accompanied by tachypnea, tachycardia, and increased local or systemic inflammation.
Etiology
- Viral respiratory infections: most common cause of AECOPD
- Rhinovirus: most common
- Others: SARS-CoV-2, influenza, RSV, parainfluenza, metapneumovirus, adenovirus
- Bacterial infections: e.g., Haemophilus influenzae, Moraxella catarrhalis, Streptococcus pneumoniae
- Risk factors for Pseudomonas aeruginosa infection include:
- Advanced COPD
- Previous hospitalizations
- Systemic glucocorticoid use
- Previous isolation of P. aeruginosa
- Risk factors for Pseudomonas aeruginosa infection include: