Epidemiology
- Second most common type of dementia (15–20% of cases)
- Prevalence increases with age (∼ 1–4% in patients ≥ 65 years).
Etiology
- VD may occur as a result of a prolonged and severe cerebral ischemia of any etiology, primarily:
- Large artery occlusion (usually cortical ischemia)
- Lacunar stroke (small vessel occlusion resulting in subcortical ischemia)
- Chronic subcortical ischemia
Pathophysiology
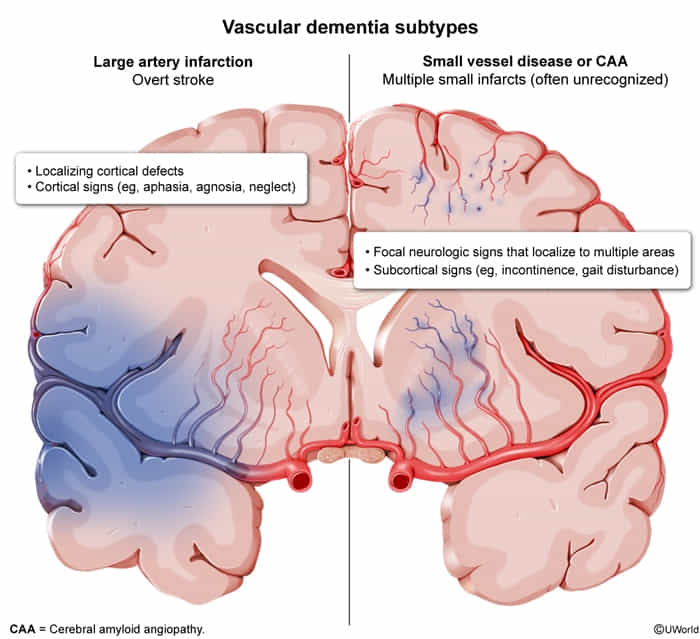
- Large-vessel atherosclerosis
- Small-vessel disease (eg, arteriolosclerosis)
- Cerebral amyloid angiopathy
Clinical features
- Cognitive decline presentation is typically abrupt and stepwise.
- Sudden decline in function after a vascular event, followed by a period of stability, then another drop.
- This contrasts with the slow, insidious progression of AD.
- Executive dysfunction is often prominent early (problems with planning, organization).
- Presence of focal neurological deficits is common and depends on the location of the infarcts (e.g., hemiparesis, visual field defects, gait disturbance, dysarthria).
- Emotional lability and mood changes can occur.
The most significant symptoms of vascular dementia tend to involve speed of thinking and problem-solving rather than memory loss.