Epidemiology
- Higher in White populations than in Black, Hispanic, or Asian populations
- Highest among individuals of Ashkenazi Jewish descent
- 15–35 years of age
Tip
Compared with Crohn disease, which is bimodal distribution with one peak at 15–35 years and another one at 55–70 years
Etiology
- Genetic predisposition (e.g., HLA-B27 association)
- Ethnicity (White populations, individuals of Ashkenazi Jewish descent)
- Protective factors: smoking
- The pathophysiology is not fully understood, as smoking has negative effects on other inflammatory diseases (e.g., Crohn disease).
Pathophysiology
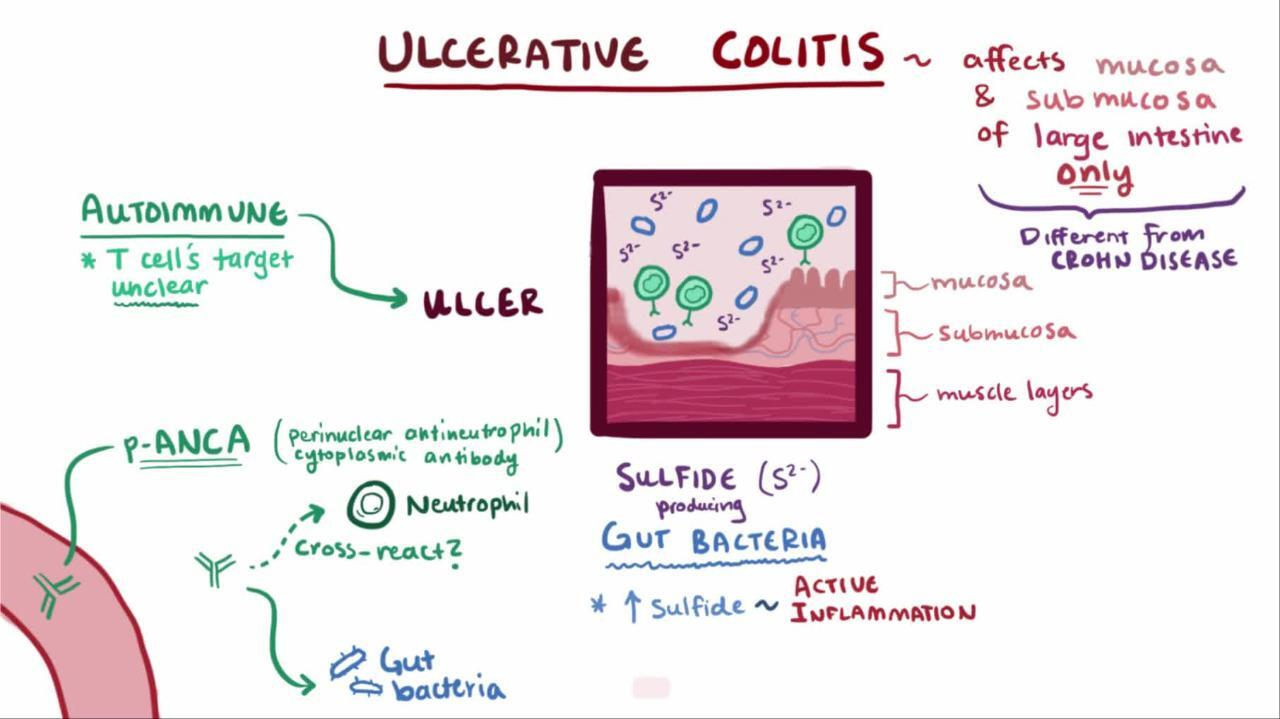
- Dysregulation of intestinal epithelium: increased permeability for luminal bacteria → activation of macrophages and dendritic cells → antigen presentation to macrophages and naive CD4+ cells
- Dysregulation of the immune system: upregulation of lymphatic cell activity (T cells, B cells, plasma cells) in bowel walls → enhanced immune reaction and cytotoxic effect on colonic epithelium → inflammation with local tissue damage (ulcerations, erosions, necrosis) in the submucosa and mucosa
- Autoantibodies (pANCA) against cells of the intestinal epithelium
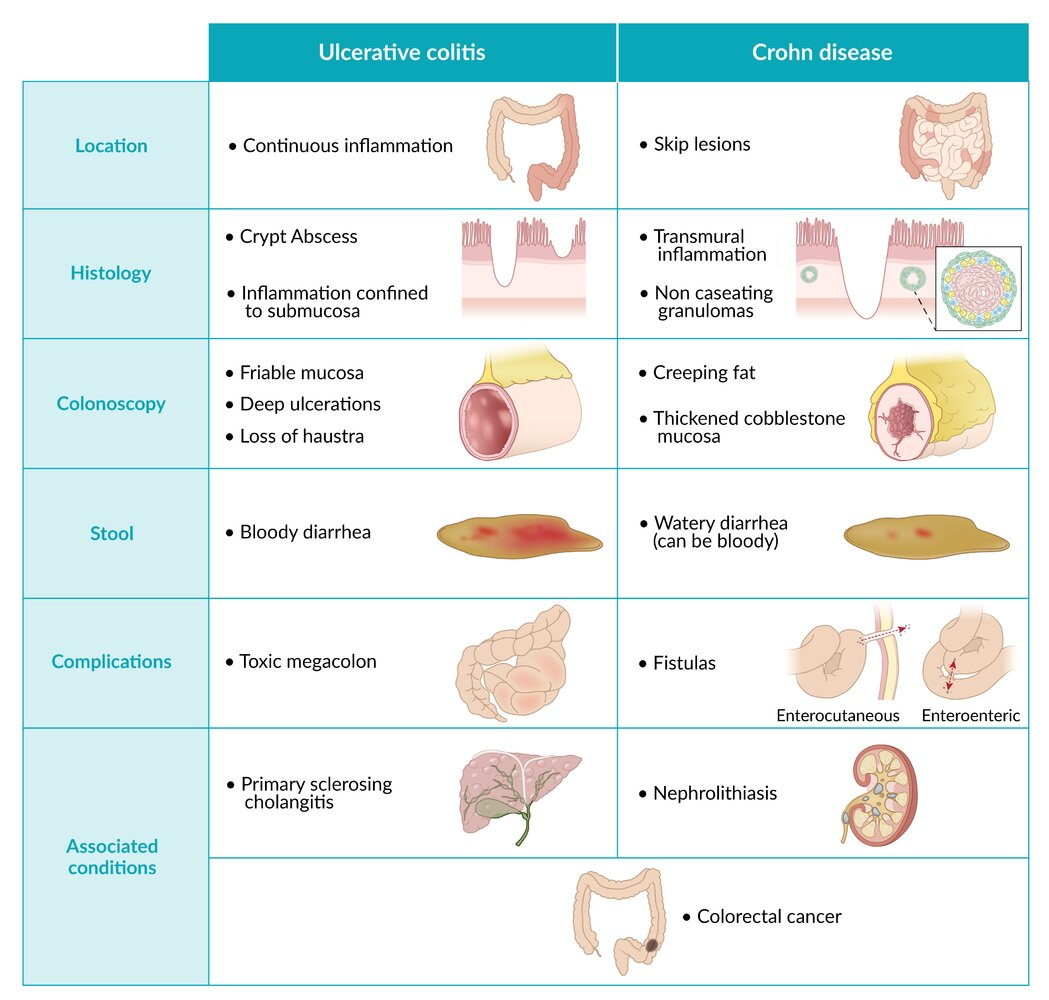
- Pattern of involvement
- Ascending inflammation that begins in the rectum and spreads continuously proximally throughout the colon
- Inflammation is limited to the mucosa and submucosa.
Crohn disease is characterized by transmural inflammation.
Unlike ulcerative colitis,
Tip
The rectum is always involved in ulcerative colitis.
Clinical features
- Intestinal symptoms
- Bloody diarrhea with mucus
- Fecal urgency
- Abdominal pain and cramps
- Tenesmus
- Extraintestinal symptoms of ulcerative colitis
- General: fatigue, fever
- Skeletal (most common extraintestinal manifestation of ulcerative colitis): osteoarthritis, ankylosing spondylitis, sacroiliitis
- Ocular: uveitis, episcleritis, iritis
- Biliary: primary sclerosing cholangitis (it is rare for patients with ulcerative colitis to develop PSC, but up to 90% of all patients with PSC will also have ulcerative colitis)
- Cutaneous
- Erythema nodosum
- Pyoderma gangrenosum
- Aphthous stomatitis
Tip
PSC is often associated with inflammatory bowel disease, especially ulcerative colitis. However, only approximately 4% of patients with inflammatory bowel disease develop PSC.
Diagnostics
Ileocolonoscopy
Recommended method for diagnosis and disease monitoring
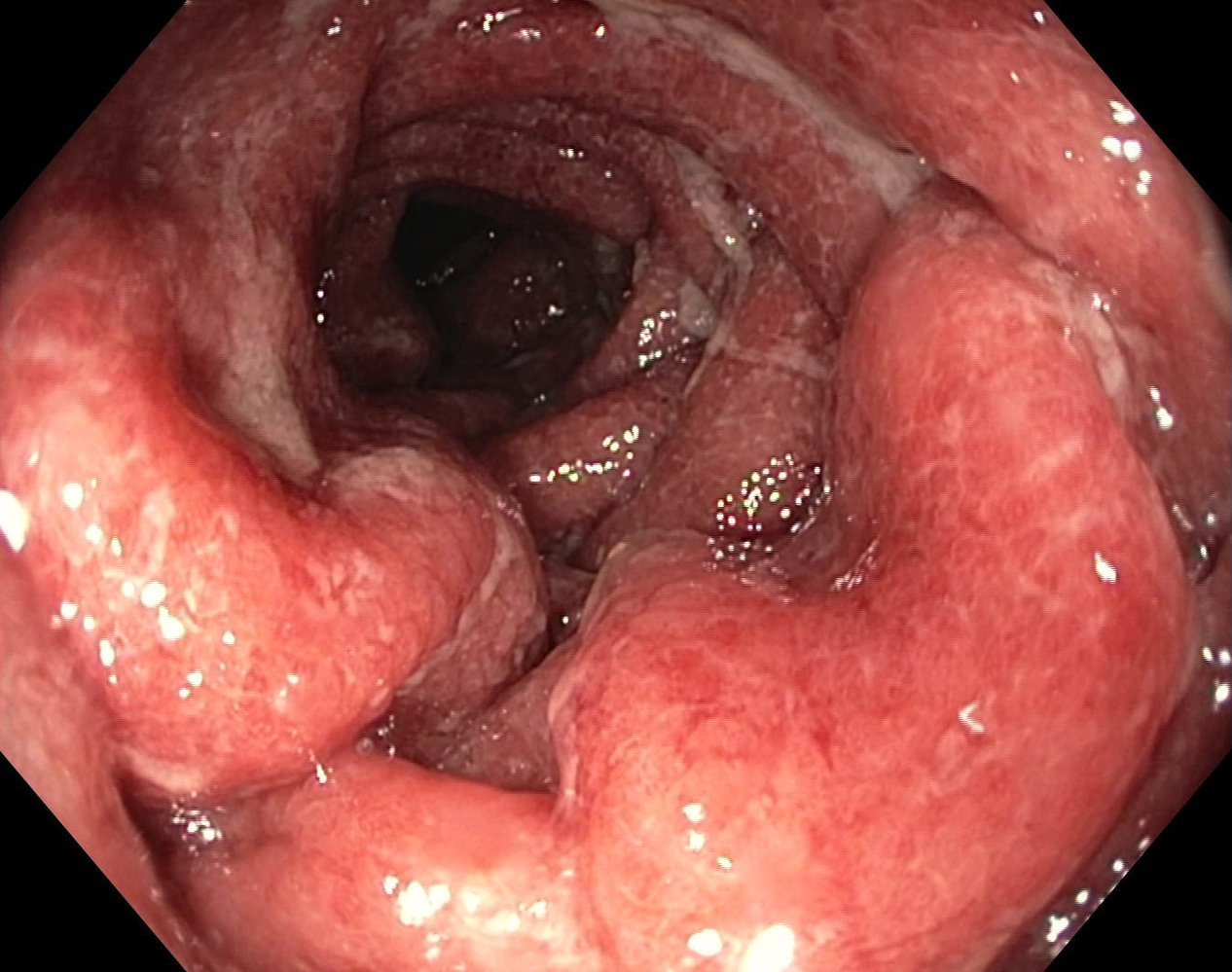
Early stages
- Inflamed, erythematous, edematous mucosa
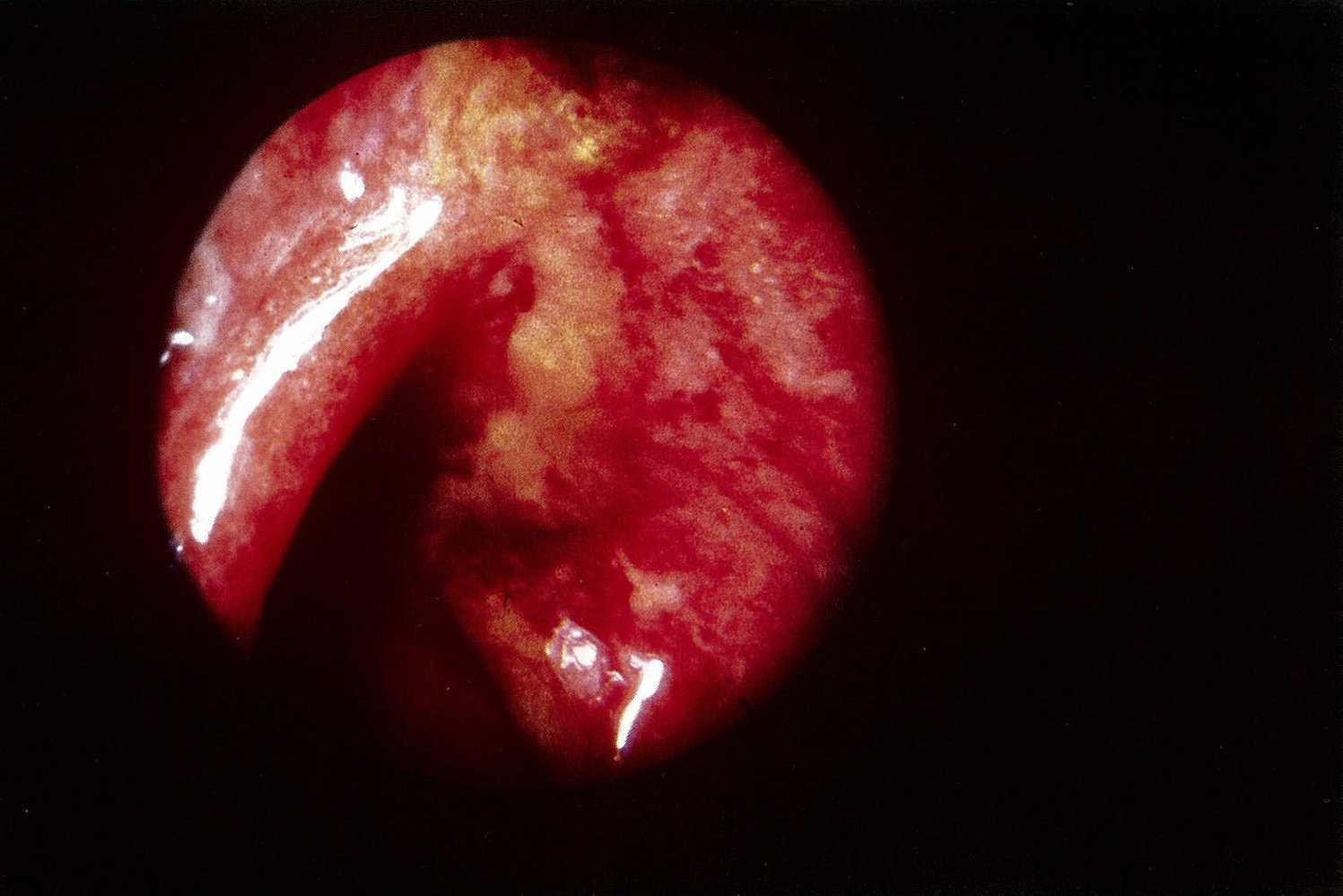
- Friable mucosa with bleeding on contact with endoscope
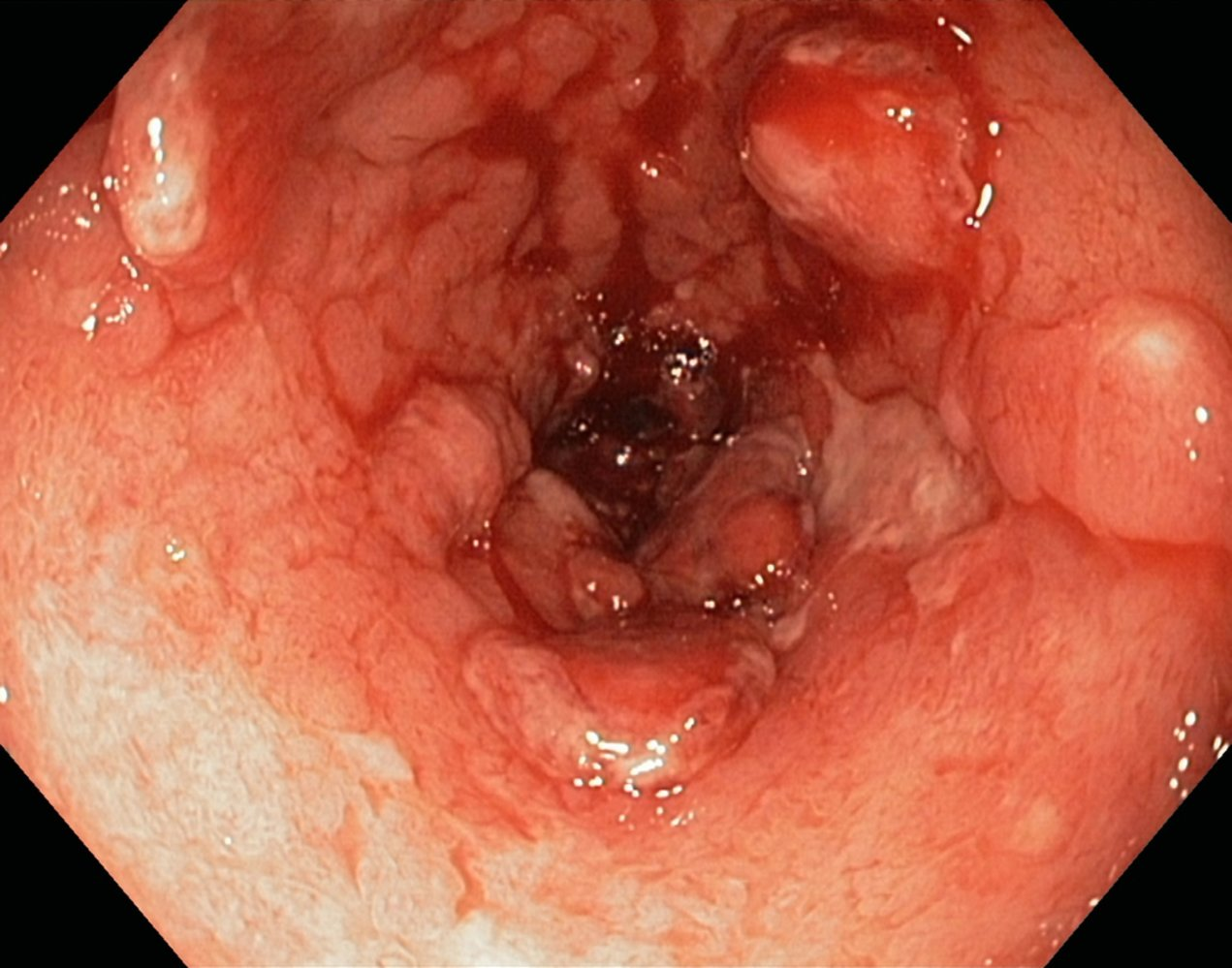 A fibrin-covered ulceration (blue overlay) and several pseudopolyps (indicated by dashed lines) are visible.
A fibrin-covered ulceration (blue overlay) and several pseudopolyps (indicated by dashed lines) are visible.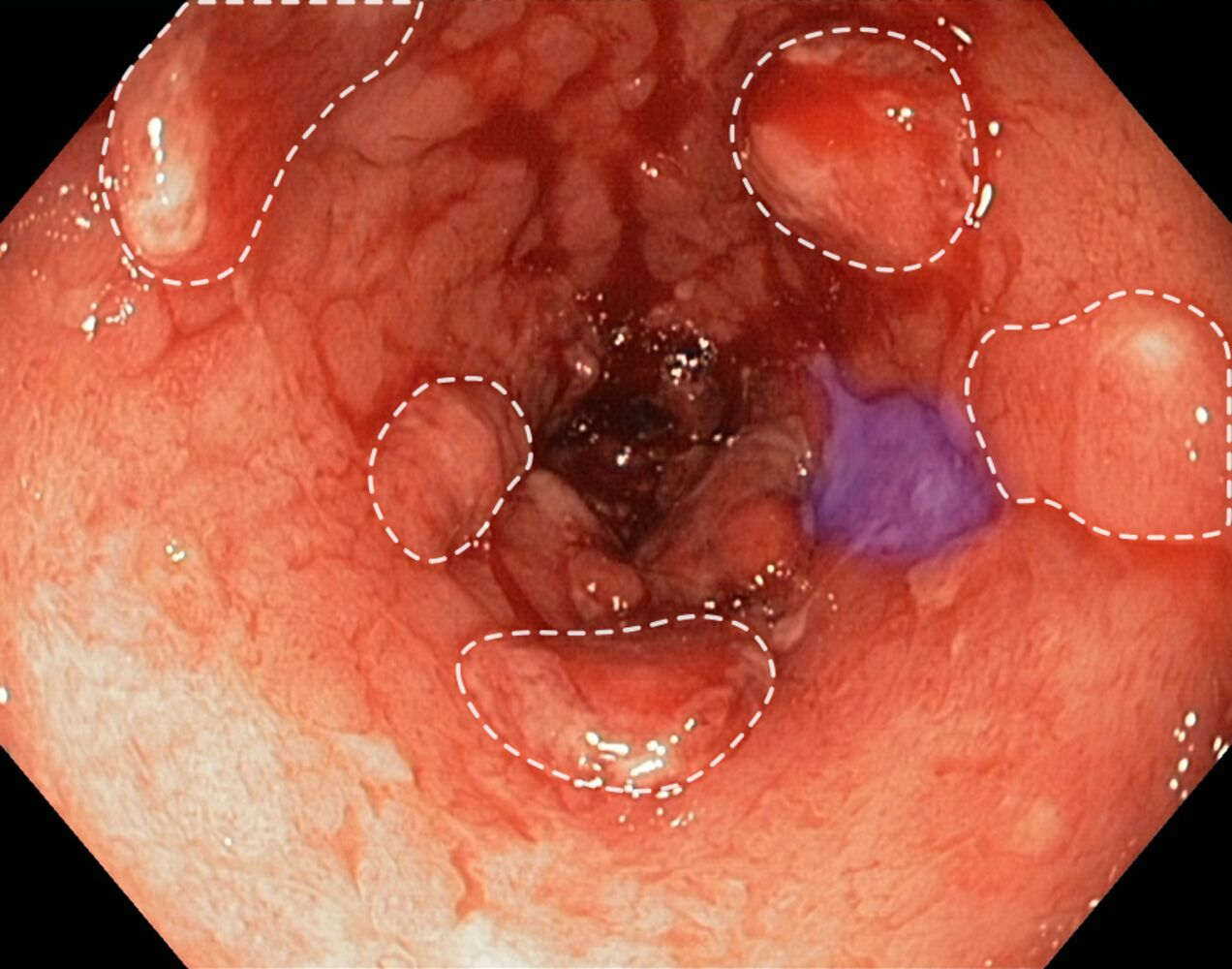
- Fibrin-covered ulcers
Chronic disease
- Loss of haustra
- Pseudopolyps
- Raised areas of normal mucosal tissue that result from repeated cycles of ulceration and healing
- Ulceration → formation of granulation tissue → deposition of granulation tissue → epithelialization

Treatment
Complications
- ↑ Risk of cancer
- chronic inflammation → hyperplasia → non-polypoid dysplasia → neoplasia
- Toxic megacolon
- Fulminant colitis
- Gastrointestinal bleeding (both acute and chronic)
- Perforation