| Feature | Stress | Urge (OAB) | Overflow |
|---|---|---|---|
| Mechanism | Urethral Hypermobility or Sphincter deficiency | Detrusor Overactivity (uninhibited spasms) | Impaired Contractility (atonic) or Obstruction |
| Symptoms | Leak w/ ↑ abd pressure (cough, sneeze, lift) | Sudden, overwhelming need to void | Constant dribbling, incomplete emptying |
| Key Risk | Multiparous women, Obesity | Elderly, MS, Idiopathic | BPH, Diabetes (neurogenic), Spinal injury |
| Diagnosis | + Bladder Stress Test (visual leak) | Clinical diagnosis | High PVR (>200mL) |
| Tx: 1st Line | Kegels (Pelvic floor training) | Bladder training | Catheterization (immediate relief) |
| Tx: Meds | (None effective) | Oxybutynin (Antimuscarinic), Mirabegron (β3-agonist) | Tamsulosin (α-blocker), Bethanechol (cholinergic) |
| Tx: Surg | Mid-urethral Sling | Botox (refractory) | TURP (if BPH) |
Mixed Incontinence: Features of both stress and urge incontinence. Very common, especially in older women. Treatment is directed at the more predominant symptom first.
Functional Incontinence: Patient has normal bladder control but cannot reach the toilet in time due to physical or cognitive impairment (e.g., dementia, severe arthritis). Management involves treating the underlying condition and using scheduled/prompted voiding.
Epidemiology
- Stress incontinence and mixed incontinence are the most common types of incontinence in female patients.
- Urge incontinence is the most common type in male patients.
Etiology
- Neurological causes
- Multiple sclerosis
- Spinal injury
- Normal pressure hydrocephalus
- Genitourinary causes
- Trauma to the pelvic floor
- Intrinsic sphincter deficiency
- Urethral hypermobility in women
- Impaired detrusor contractility
- Bladder outlet obstruction
- Pelvic floor weakness
- Transient causes of urinary incontinence
- Drugs (e.g., diuretics)
- Urinary tract infections
- Postmenopausal atrophic urethritis
- Psychiatric causes (especially depression, delirium/confused state)
- Excessive urinary output (in conditions like hyperglycemia, hypercalcemia, CHF)
- Stool impaction
- General risk factors
- Recurrent urinary tract infections
urethritis/vaginitis, Pharmaceutical, Psychiatric causes (especially depression), Excessive urinary output (hyperglycemia, hypercalcemia, CHF), Restricted mobility, Stool impaction.
To remember the reversible causes of acute urinary incontinence, think DIAPPERS: Delirium/confusion, Infection, Atrophic
Classifications
Overflow incontinence
Mechanism
- Impaired (weak) detrusor contractility
- Bladder outlet obstruction (e.g., BPH)
- Both mechanisms can lead to incomplete bladder emptying → bladder overfilling → chronically distended bladder with ↑ bladder pressure → dribbling of urine (leak) when intravesical pressure > outlet resistance
Clinical features
- Frequent, involuntary intermittent/continuous dribbling of urine in the absence of an urge to urinate
- Occurs only when the bladder is full
- Postvoid residual urine volume (seen on ultrasound or with catherization)
- Assess for urinary retention via bladder scan (≥200 mL) or straight catheterization yielding ≥200 mL urine output.
Treatment
- Urinary catheter: for scheduled bladder emptying
- Intermittent → prevention of catheter-associated UTIs and is favored by most patients; indwelling catheters may be considered if necessary.
Stress incontinence
Epidemiology
Prevalence increases with age.
Etiology
- Pathomechanism: outlet incompetence
- Urethral hypermobility: loss of pelvic floor musculature and/or connective tissue support → weak pelvic floor → inability of the urethra to completely close
- Intrinsic sphincter deficiency
- Risk factors
Pathophysiology
Clinical features
- Physical activity that causes increased intra-abdominal pressure (e.g., laughing, sneezing, coughing, exercising) leads to loss of urine
- Frequent, predictable, small-volume urine losses with no urge to urinate prior to the leakage
Diagnostics
Treatment
Conservative treatment
- Kegel exercises
- Strengthen Levator ani
- Lifestyle changes (e.g., weight loss, avoiding alcohol and caffeine, smoking cessation)
- Vaginal pessary
Surgical procedures
- Indicated if conservative treatment does not provide sufficient improvement of symptoms
- Procedure of choice: midurethral sling to elevate the urethra
Link to original
Stress incontinence
Epidemiology
Prevalence increases with age.
Etiology
- Pathomechanism: outlet incompetence
- Urethral hypermobility: loss of pelvic floor musculature and/or connective tissue support → weak pelvic floor → inability of the urethra to completely close
- Intrinsic sphincter deficiency
- Risk factors
Pathophysiology
Clinical features
- Physical activity that causes increased intra-abdominal pressure (e.g., laughing, sneezing, coughing, exercising) leads to loss of urine
- Frequent, predictable, small-volume urine losses with no urge to urinate prior to the leakage
Diagnostics
Treatment
Conservative treatment
- Kegel exercises
- Strengthen Levator ani
- Lifestyle changes (e.g., weight loss, avoiding alcohol and caffeine, smoking cessation)
- Vaginal pessary
Surgical procedures
- Indicated if conservative treatment does not provide sufficient improvement of symptoms
- Procedure of choice: midurethral sling to elevate the urethra
Link to original
Urge incontinence
Epidemiology
Prevalence increases with age
Etiology
The condition is caused by sensory or motor dysfunction.
- Idiopathic (most common)
- Neurological conditions
Pathophysiology
Inflammatory conditions (e.g., UTI) or neurogenic disorders → sphincter dysfunction, detrusor overactivity, or overactive bladder → autonomous contractions of the detrusor muscle and premature initiation of a normal micturition reflex
Clinical features
- Urinary urgency: sudden urge to urinate
- Loss of urine without exertion, with urinary tenesmus → frequent episodes, with variable volumes of urine voided each time
Diagnostics
Treatment
Mnemonic
Oxybutynin treats Overactive bladder.
Link to original
Urge incontinence
Epidemiology
Prevalence increases with age
Etiology
The condition is caused by sensory or motor dysfunction.
- Idiopathic (most common)
- Neurological conditions
Pathophysiology
Inflammatory conditions (e.g., UTI) or neurogenic disorders → sphincter dysfunction, detrusor overactivity, or overactive bladder → autonomous contractions of the detrusor muscle and premature initiation of a normal micturition reflex
Clinical features
- Urinary urgency: sudden urge to urinate
- Loss of urine without exertion, with urinary tenesmus → frequent episodes, with variable volumes of urine voided each time
Diagnostics
Treatment
Mnemonic
Oxybutynin treats Overactive bladder.
Link to original
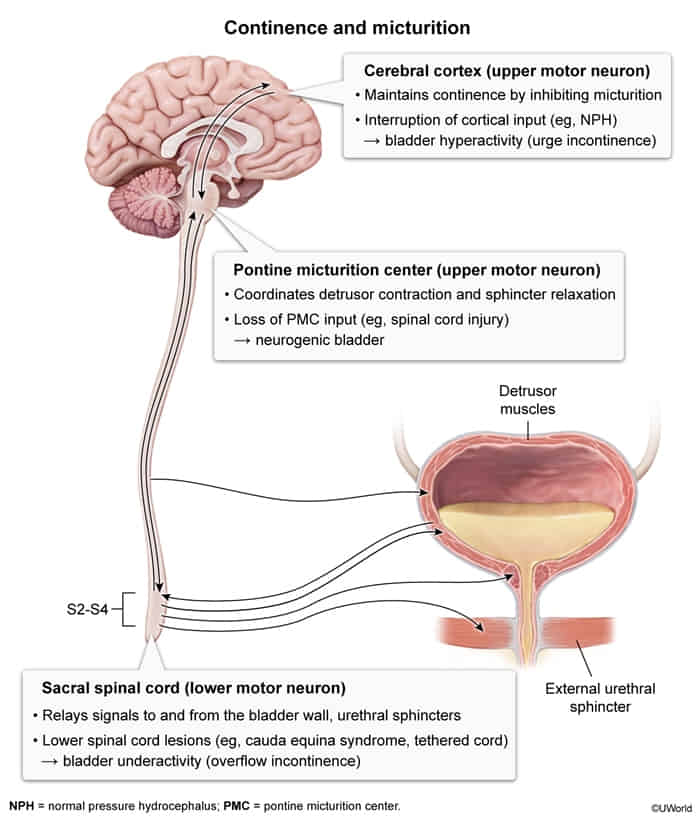
Neurogenic bladder dysfunction
Mechanism
detrusor sphincter dyssynergia
- Simultaneous contractions of the detrusor muscle and involuntary activation of the urethral sphincter → blockage of bladder outlet → small amounts of urine are pressed through the contracted sphincter muscle → high intravesical pressure along with inappropriate contraction of the urethral sphincter
- Commonly seen in multiple sclerosis and spinal cord injury
Clinical features
- Voiding and/or storage dysfunction, intermittent voiding, urinary retention
- Irregular, small volume incontinence without an associated urge to void (sometimes referred to as reflex incontinence)
Total incontinence
Complete loss of sphincter function (due to previous surgery, nerve damage, metastasis) → Urinary leakage occurs at all times
Clinical features
Diagnostics
Treatment
Autonomic & Somatic Innervation
- Sympathetic (Storage/“Sympathetic Stores”): Hypogastric nerve (T11-L2).
- Relaxes detrusor muscle (via β3 receptors) → allows filling.
- Contracts internal urethral sphincter (via α1 receptors) → prevents leakage.
- Parasympathetic (Peeing/Voiding): Pelvic splanchnic nerves (S2-S4).
- Contracts detrusor muscle (via M3 receptors) → initiates emptying.
- Relaxes internal urethral sphincter (via M3 receptors).
- Somatic (Voluntary Control): Pudendal nerve (S2-S4).
- Contracts external urethral sphincter (via Nicotinic receptors) → allows voluntary holding of urine.
Overview of pharmacotherapy
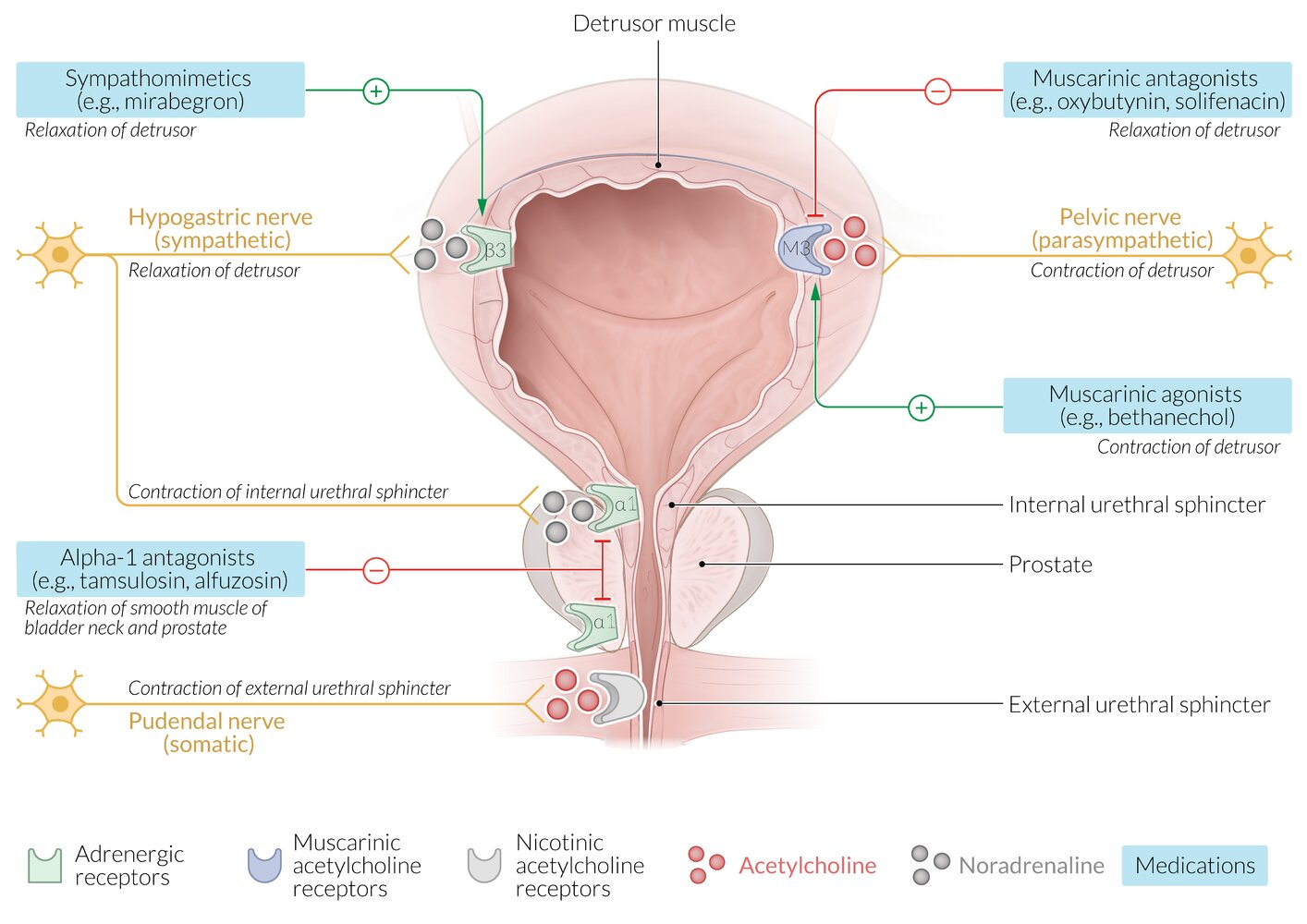
Warning
The use of muscarinic agonists may lead to urinary urgency, while the use of sympathomimetics or muscarinic antagonists may lead to urinary retention, especially if there is an untreated outlet obstruction.
Tip
No pharmacological therapies are FDA-approved for stress incontinence; treatment is primarily conservative with surgery.