Epidemiology
Etiology
Common causes of PUD
The two major contributing factors to the development of PUD are gastrointestinal infection with H. pylori and nonsteroidal anti-inflammatory drug (NSAID) use.
- Helicobacter pylori infection
- Associated with 40–70% of duodenal ulcers and 25–50% of gastric ulcers
- Chronic NSAID use
Tip
Unlike aspirin and other NSAIDS, acetaminophen is believed to be safe for people with ulcers. It is inactivated peripherally. Since it doesn’t thin the blood, it doesn’t increase the risk of bleeding either.
Associated risk factors
- Shared risk factors for PUD, GERD and gastritis (i.e., smoking, heavy alcohol use, glucocorticoids, caffeine)
Rare causes of PUD
- Acid hypersecretory states
Pathophysiology
- H. pylori
- Gastric ulcers
- H. pylori colonizes the gastric body (corpus)
- H. pylori secretes urease → conversion of urea to NH3 → alkalinization of acidic environment → survival of bacteria in gastric lumen
- Bacterial colonization and attachment to epithelial cells → release of cytotoxins (e.g., cagA toxin) → disruption of the mucosal barrier and damage to underlying cells
- Duodenal ulcers
- H. pylori colonizes the gastric antrum, see Stomach histology
- H. pylori inhibits somatostatin secretion → ↑ gastrin secretion → ↑ H+ secretion → excess H+ delivery to the duodenum
- Direct spread of H. pylori to the duodenum → inhibition of duodenal HCO3- secretion→ acidification and insufficient neutralization of duodenal contents
- Gastric ulcers
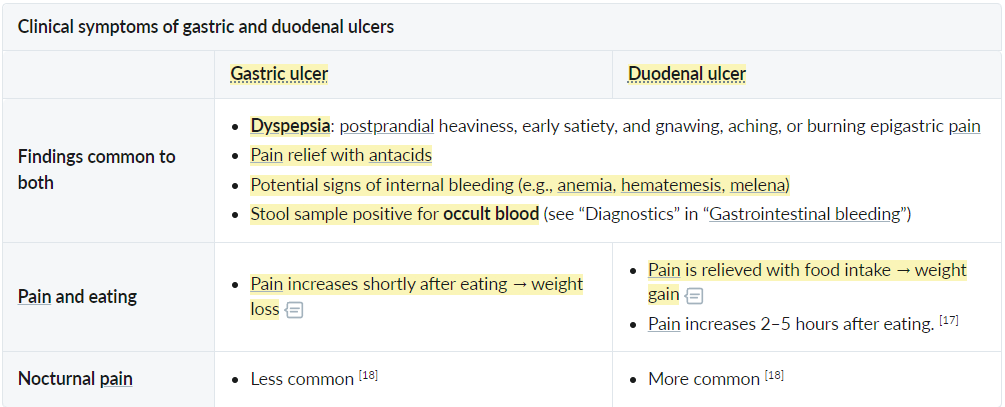
Clinical features
Diagnostics
Initial tests
- Noninvasive: Order one of the following if EGD is not indicated.
- Urea breath test: The labeled carbon isotope in a breath sample is quantified.
- H. pylori stool antigen test: detects H. pylori antigens via an enzyme immunoassay
- Invasive: Order one or both of the following tests (performed on a gastric biopsy sample) for patients with indications for EGD.
- Histology (gold standard)
- Staining and direct microscopic identification
- Typical microscopic appearance of H. pylori: curved, gram-negative rods with multiple flagella
- Sensitivity and specificity are not affected by recent PPI treatment.
- Rapid urease test: detects the amount of ammonia produced by H. pylori during urea hydrolysis
- The rapid urease test is an indirect test for H pylori based on bacterial production of the enzyme urease, which splits gastric urea into ammonia and CO2. During the test, biopsy specimens are exposed to a solution containing urea and a pH indicator such as phenol red, which changes color from yellow to pink at alkaline pH. A color change indicates the presence of bacterial urease and confirms active H pylori infection.
- Histology (gold standard)
Indications for biopsy
- Gastric ulcers
- Biopsies are recommended in most cases.
- Multiple biopsies are recommended.
- From the edge and base of the ulcer (essential to rule out malignancy, which is not uncommon in gastric ulcers)
- The central part of the ulcer may contain necrotic tissue, fibrin slough, and other debris, which are typically not useful for diagnostic purposes.
- Multiple biopsies from different areas of the stomach lining, including those not surrounding the ulcer (to test for H. pylori)
- Duodenal ulcers
- Obtain biopsies from ulcers with endoscopic features that suggest malignancy.
- Duodenal ulcers are usually benign and do not require routine biopsy.
Treatment
Complications
Bleeding peptic ulcer
- Etiology
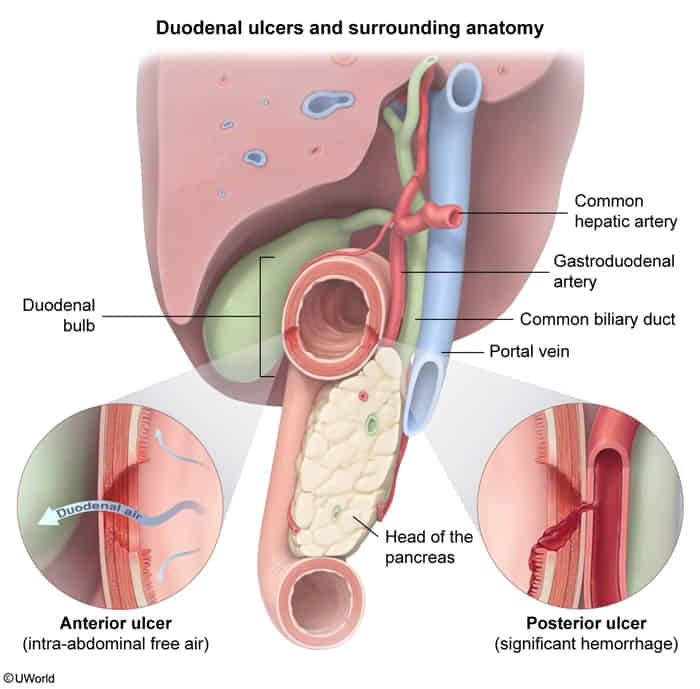
- Posterior duodenal ulcers are more likely to bleed than anterior duodenal ulcers.
- Gastric ulcers of the lesser curvature may cause bleeding from the left gastric artery.
- Duodenal ulcers of the posterior wall may cause bleeding from the gastroduodenal artery.
Peptic ulcer perforation
- Definition: full-thickness injury and loss of bowel wall integrity that results in leakage of gastrointestinal contents
- The second most common complication of PUD
- PUD is the most common cause of GI perforation.
- Etiology
- Prepyloric gastric ulcers are the most common cause of perforation.
- Duodenal ulcers of the anterior wall are more likely to perforate than ulcers of the posterior wall.
- This is because less protection is provided by the surrounding anatomical structures.
- Clinical features
- Sudden, diffuse abdominal pain and rigidity
- Fever, tachycardia, tachypnea, hypotension
- Pneumoperitoneum
- Shoulder pain (irritation of the phrenic nerve)