An acquired genetic defect of the hematopoietic stem cell characterized by a triad of hemolytic anemia, pancytopenia, and thrombosis
Epidemiology
Etiology
Pathophysiology
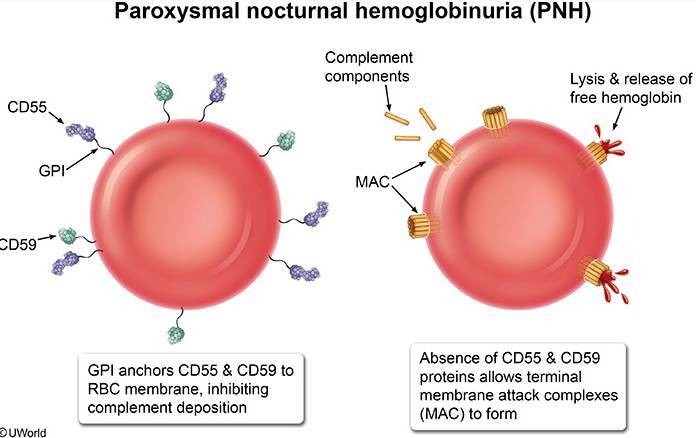
- Physiologically, a membrane-bound glycosylphosphatidylinositol (GPI) anchor protects RBCs against complement-mediated hemolysis.
- Acquired mutation on the PIGA gene located on the X chromosome → GPI anchor loses its protective effect → RBC destruction by complement and reticuloendothelial system → intravascular and extravascular hemolysis
- The GPI anchor proteins involved in PNH are:
- CD55/DAF (Decay-accelerating factor)
- CD59/MIRL (Membrane inhibitor of reactive lysis)
- PNH can also occur in patients with aplastic anemia and MDS.
- Autoimmunity to HSCs, causing bone marrow failure → pancytopenia
Clinical features
- Pallor, excessive fatigue, weakness
- Intermittent jaundice
- Episodes of hemoglobinuria causing pink/red/dark urine which usually occurs in the morning due to the concentration of urine overnight.
- Vasoconstriction
- The scavenging of nitric oxide by free Hb results in smooth muscle contraction.
- Headache, pulmonary hypertension
- Abdominal pain, dysphagia, erectile dysfunction
- Venous thrombosis in unusual locations (e.g., hepatic, cerebral, and/or abdominal veins)
- Hemolysis generates free Hb, which scavenges serum nitric oxide (a vasodilator), causing vasoconstriction.
- Free Hb also promotes oxidative stress, which activates the endothelium of blood vessels, inducing platelet aggregation.
- Increased risk of infections (in case of pancytopenia)
Diagnostics
- CBC: anemia, thrombocytopenia, and/or pancytopenia ; usually ↑ reticulocytes
- Hemolysis workup: ↓ haptoglobin
- Direct Coombs test: negative
- complement-mediated RBC destruction
- Flow cytometry of peripheral blood (confirmatory test for PNH): can show deficiency of GPI-linked proteins on the surface of RBCs and WBCs (e.g., CD55, CD59)