Pathophysiology
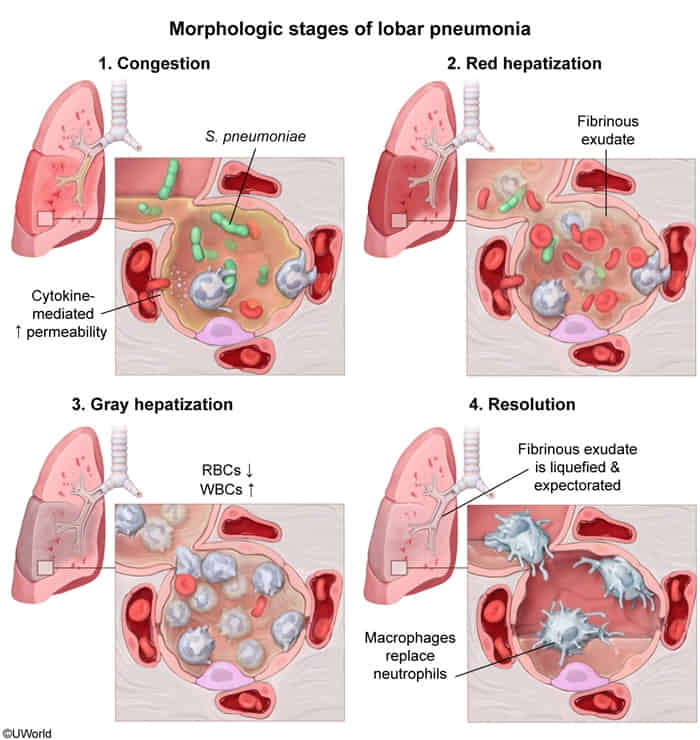
Pattern of involvement
- Classic (typical) pneumonia of an entire lobe; primarily caused by pneumococci
- Characterized by inflammatory intra-alveolar exudate, resulting in consolidation
- Can involve the entire lobe or the whole lung
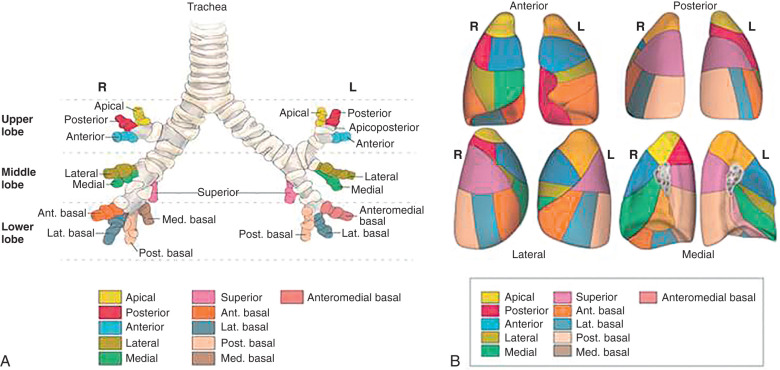
- Bronchopneumonia: mostly commonly a descending infection that affects the bronchioles and adjacent alveoli
- Primarily caused by pneumococci and/or other streptococci
- Characterized by acute inflammatory infiltrates that fill the bronchioles and the adjacent alveoli (patchy distribution)
- Usually involves the lower lobes or right middle lobe and affects ≥ 1 lobe
- Manifests as typical pneumonia
- Necrotizing bronchopneumonia and pneumatocele are caused by Staphylococcus aureus and are often preceded by an influenza infection.
- Interstitial pneumonia: interstitial inflammation, typically caused by Mycoplasma and viral infections
- Characterized by a diffuse patchy inflammation that mainly involves the alveolar interstitial cells
- Bilateral multifocal opacities are classically found on chest x-ray.
- Manifests as atypical pneumonia
- Often has an indolent course (walking pneumonia)
- Miliary pneumonia: multiple small infiltrations caused by hematogenous dissemination (e.g., of tuberculosis)
- Cryptogenic organizing pneumonia: characterized by inflammation of the bronchioles and surrounding structures
Clinical features
Typical pneumonia
Typical pneumonia is characterized by a sudden onset of symptoms caused by lobar infiltration.
- Severe malaise
- High fever and chills
- Productive cough with purulent sputum (yellow-greenish)
- Crackles and bronchial breath sounds on auscultation
- Decreased breath sounds
- Enhanced bronchophony, egophony, and tactile fremitus
- Dullness on percussion
- Tachypnea and dyspnea (nasal flaring, thoracic retractions)
Suspect bacterial pneumonia in immunocompromised patients with acute high fever and pleural effusion.
Atypical pneumonia
Atypical pneumonia typically has an indolent course (slow onset) and commonly manifests with extrapulmonary symptoms.
- Nonproductive, dry cough
- Dyspnea
- Auscultation often unremarkable
- Common extrapulmonary features include fatigue, headaches, sore throat, myalgias, and malaise.
This classification does not have a major impact on patient management because it is not always possible to clearly distinguish between typical and atypical pneumonia.
Pathogen-specific pneumonia
Mycoplasma pneumonia
Microbiology
- Incomplete/absent cell wall (not visible on gram stain)
- Bacterial membrane stabilized by cholesterol (obtained from host cell)
- Grows on Eaton agar → “fried egg” appearance
Epidemiology
- One of the most common causes of atypical pneumonia
- More common in school-aged children and adolescents
- Outbreaks most commonly occur in schools, colleges, prisons, and military facilities.
Clinical features
- Causes “atypical” or “walking” pneumonia.
- Characterized by an insidious onset of low-grade fever, headache, malaise, and a persistent, non-productive, hacking cough.
- Pharyngitis is common. Bullous myringitis (inflammation of the eardrum) is a classic but rare finding.
- The clinical picture is often milder than the chest X-ray findings would suggest.
- Primarily affects children and young adults (<30 years old).
- Extrapulmonary Manifestations (High-Yield Associations)
- M. pneumoniae infection can cause a wide range of non-respiratory symptoms, which may occur even without significant respiratory illness.
- Hematologic: Cold agglutinin autoimmune hemolytic anemia.
- Dermatologic: Erythema multiforme, Stevens-Johnson Syndrome (SJS), and nonspecific maculopapular rashes.
- Neurologic: Encephalitis, Guillain-Barré syndrome, and aseptic meningitis.
- Cardiac: Myocarditis and pericarditis.
- Musculoskeletal: Arthralgias.
Diagnostics
- CXR: Typically shows patchy or diffuse interstitial infiltrates, often more prominent in the lower lobes. The X-ray often appears worse than the patient’s clinical state.
- Labs:
- WBC count is often normal.
- Cold agglutinins (IgM): A classic finding in about 50% of patients. These IgM antibodies bind to the I antigen on RBCs at cold temperatures, causing agglutination and sometimes a mild autoimmune hemolytic anemia. The titer peaks 2-3 weeks after infection onset.
- Definitive Dx: Serology or PCR is the most sensitive and specific method for diagnosis. Culture is difficult and slow, requiring special media (Eaton agar).
Aspiration pneumonia
Definitions
- Aspiration pneumonia: a type of pneumonia that occurs as a result of upper airway or stomach microbes (anaerobes) aspiration
- Aspiration pneumonitis
- Aspiration of gastric acid that initially causes tracheobronchitis, with rapid progression to chemical pneumonitis
- May cause ARDS in extreme cases
Etiology
- Gram-positive and gram-negative aerobic bacteria predominate in community-acquired infections (e.g., S. pneumonia, S. aureus, H. influenza, Enterobacteriaceae).
- Gram-negative bacilli predominate in hospital-acquired infections (e.g., P. aeruginosa, Klebsiella spp.).
- Mixed infections with anaerobic organisms may occur (e.g., Fusobacterium, Peptostreptococcus, Bacteroides).
Clinical features
- Aspiration pneumonitis
- Present hours after aspiration event
- Range from no symptoms to nonproductive cough, ↓ O2, respiratory distress
- CXR infiltrates (one or both lower lobes) resolve without antibiotics
- Aspiration pneumonia
- Present days after aspiration event
- Fever, cough, ↑ sputum
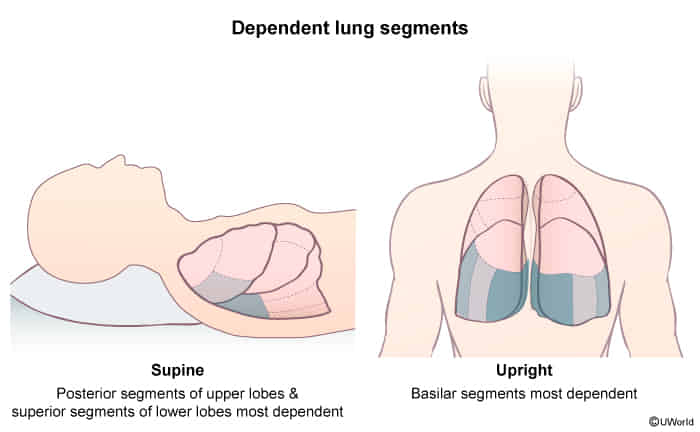
- CXR infiltrate in dependent lung segment (classically RLL)
- Can progress to abscess
Diagnostics
Imaging: The lung region in which the infiltrates are seen depends on the patient’s position on aspiration.
- Supine position: posterior segments of the upper lobes and the superior segments of the lower lobes (most common site of aspiration)
- Standing/sitting: posterior basal segment of the right lower lobe
- Right lateral decubitus position: posterior segment of the right upper lobe or right middle lobe
Mnemonic
Inhale a bite, goes down the right