Etiology
Pathogens
- Escherichia coli: leading cause of UTI (approx. 80%)
- Ten times more common in females (shorter urethras colonized by fecal microbiota).
- Staphylococcus saprophyticus: 2nd leading cause of UTI in sexually active women
- Klebsiella pneumoniae: 3rd leading cause of UTI
- Proteus mirabilis
- Produces ammonia, giving the urine a pungent or irritating smell
- Associated with struvite stone formation
- Nosocomial bacteria: Serratia marcescens, Enterococci spp., and Pseudomonas aeruginosa are associated with increased drug resistance.
Tip
- Urethritis is often caused by sexually transmitted infections (STIs), e.g. N gonorrhoeae.
- UTIs are generally caused by bacteria from the gastrointestinal tract, e.g. E coli.
Pathophysiology
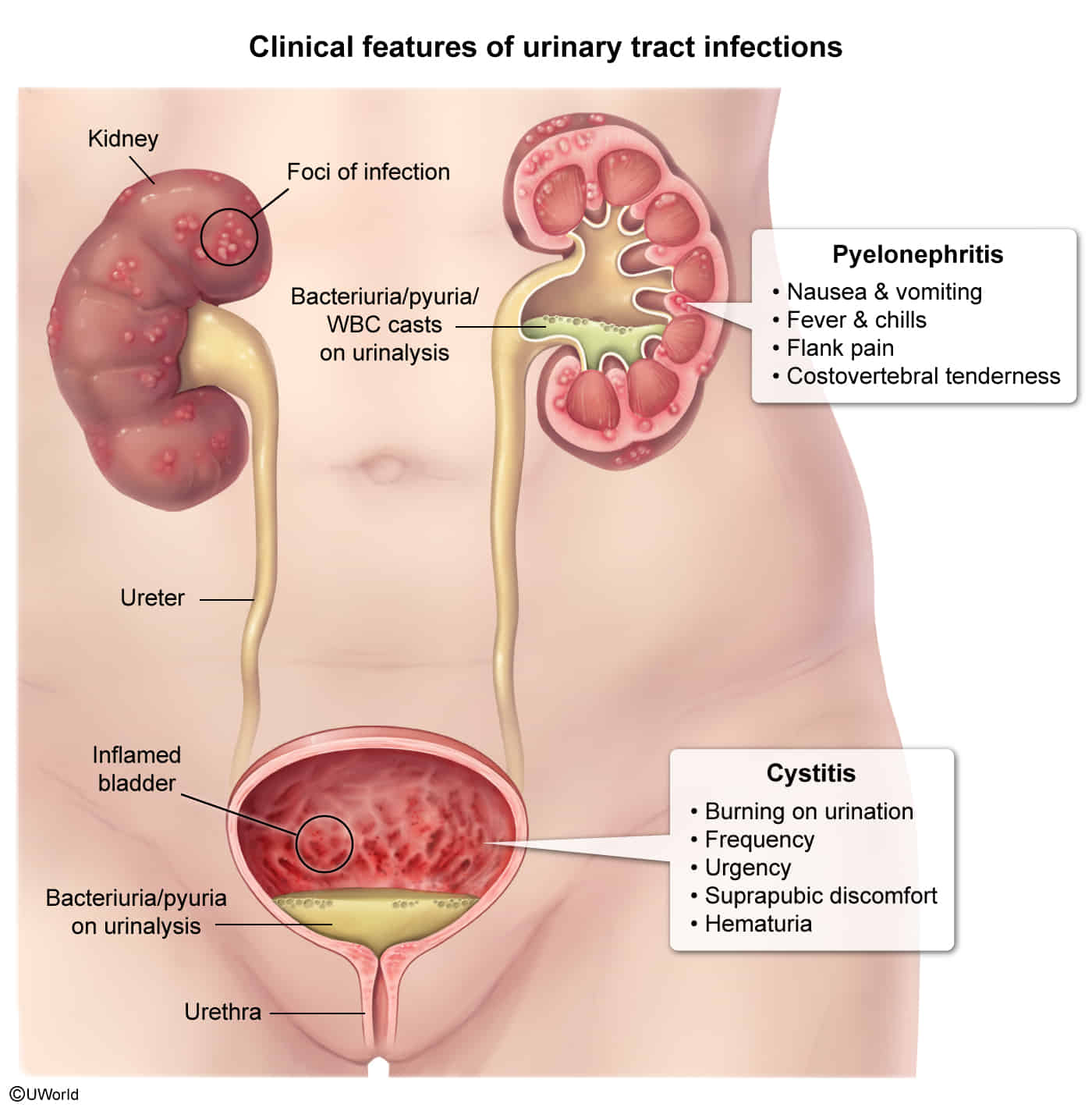
Clinical features
Diagnostics
Urinalysis
- Pyuria: presence of white blood cells (WBCs) in the urine
- Positive leukocyte esterase: an enzyme produced by WBC
- ≥ 5 WBC/HPF
- Bacteriuria: presence of bacteria in the urine
- Positive urinary nitrites: indicate bacteria that convert nitrates to nitrites (most commonly gram-negative bacteria; e.g., E.coli, Klebsiella, Proteus mirabilis)
- Other findings
- Leukocyte casts may indicate pyelonephritis.
- Micro- or macroscopic hematuria may be present.
- Alkaline urine (pH > 8) and struvite crystals in sediment: indicate urease-producing organisms (e.g., Proteus, Klebsiella, Staphylococcus saprophyticus)
Transclude of Drawing-2025-03-29-16.01.03.excalidraw
Treatment
UTI in pregnancy
- Pregnancy may increase the risk of recurrent bacteriuria and UTIs.
- Treatment
- Empiric antibiotics for ASB and lower UTI considered appropriate during pregnancy include:
- Fosfomycin
- Beta-lactam antibiotics for 5–7 days
- Oral cephalosporins (e.g., cefpodoxime)
- Aminopenicillins plus beta-lactamase inhibitors (e.g., amoxicillin/clavulanic acid)
- Empiric antibiotics for ASB and lower UTI considered appropriate during pregnancy include:
Catheter-associated UTI (CAUTI)
- Definitions
- Catheter-associated UTI (CAUTI): symptomatic UTI occurring in a patient with an indwelling urinary catheter OR within 48 hours after removal of a urinary catheter
- Catheter-associated asymptomatic bacteriuria (CAASB): bacteriuria (≥ 105CFU/mL) without symptoms in a patient with an indwelling urinary catheter OR within 48 hours after removal of a urinary catheter
- Risk factors
- Duration of catheter use, especially >48 hr (most important)
- Female sex
- Advanced age
- Diabetes mellitus
- Treatment
- Catheter removal or replacement
- Remove if no longer necessary.
- Replace if still necessary and present for > 2 weeks.
- Antibiotic therapy
- Guided by culture results and local resistance patterns
- Duration: typically 7–14 days depending on the resolution of symptoms
- Catheter removal or replacement