Epidemiology
- Opioid overdose is the most common cause of drug overdose death.
Etiology
Indications
Pain management
- Buprenorphine
- Partial μ-agonist
- Chronic pain refractory to nonopioid analgesics: transdermal patches
- Management of opioid use disorder (sublingual and subcutaneous preparations)
- Other features
- Can displace other opioids from opioid receptors due to high receptor affinity and precipitate withdrawal since it does not produce the same receptor activation as a full agonist
- High doses of naloxone or naltrexone are necessary to antagonize buprenorphine effects.
Strategies for safe opioid prescribing
- Optimize non-opioid interventions
- Use acetaminophen/NSAIDs, supportive care (eg, heat/ice) for mild/moderate pain
- Avoid routine opioid use for chronic pain
- Optimize opioid dose and duration
- Limit therapy to <5 days for acute pain
- Use lowest dose resulting in adequate pain control
- Avoid long-acting opioids
- Optimize monitoring
- Counsel patients on safe use; arrange close follow-up
- Educate patients on safe disposal of unused opioids
Clinical features
Opioid toxidrome
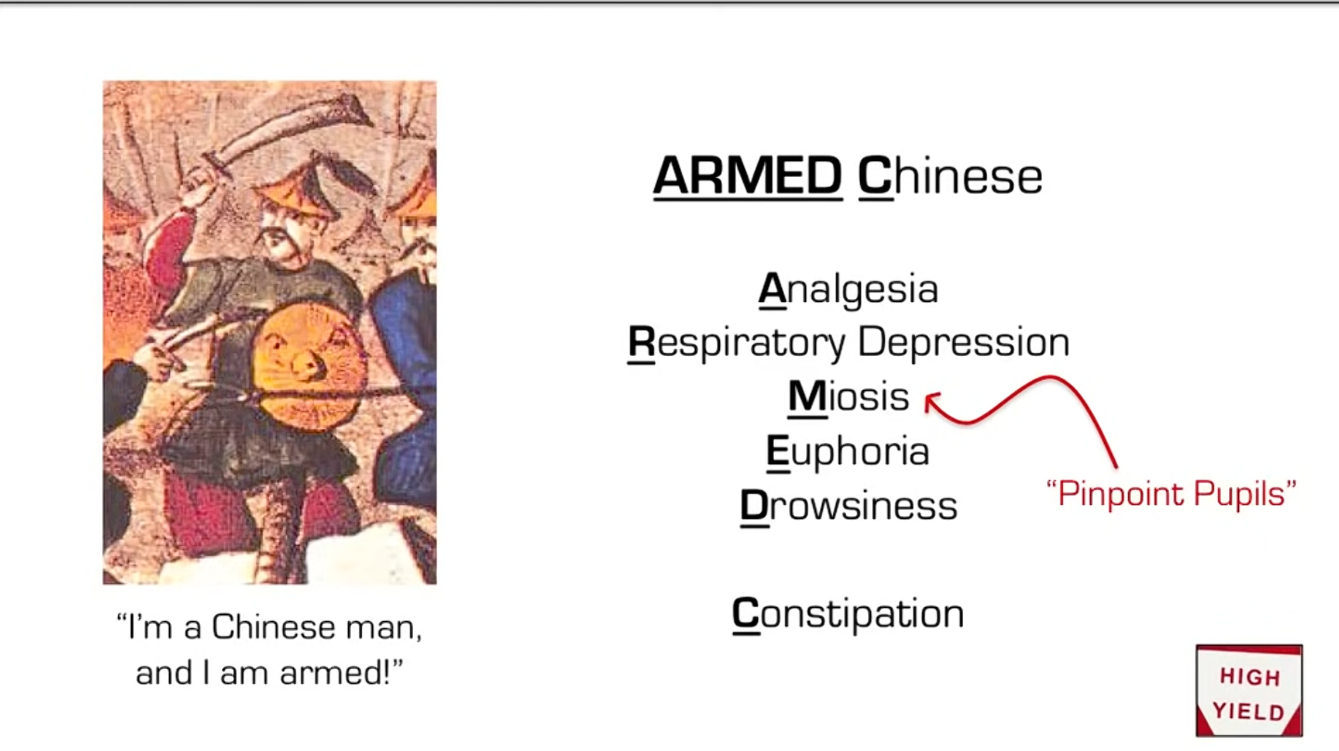 The classic triad consists of:
The classic triad consists of:
- Altered mental status (e.g., CNS depression, euphoria)
- Bilateral miosis (pinpoint pupils)
- Opioid-induced respiratory depression
Warning
The absence of miosis does not rule out opioid overdose as hypoxia, co-ingested drugs (e.g., cocaine, amphetamines), and/or medications (e.g., atropine) may cause mydriasis, thereby counteracting the miotic effect of opioids.
Opioid-induced respiratory depression (OIRD)
- ↓ Respiratory rate and/or apnea
- ↓ Tidal volume
Warning
OIRD is the most common cause of death from opioid overdose and is treated with naloxone for opioid overdose.
Other clinical features
Diagnostics
Treatment
Tip
Naloxone has short half-life (60 minutes on average; ranges from 30 to 90 minutes). Therefore, patients may develop recurrent symptoms of opioid toxicity after naloxone is metabolized, and frequent redosing may be necessary.
- Naloxone
- A competitive opioid receptor antagonist with high binding affinity to thejas a relatively short duration of action, which can lead to renewed effect of opioids.
- Naltrexone
- Maintenance therapy for patients who have completed opioid withdrawal and want to abstain from opioid use