- Description
- Pancytopenia caused by bone marrow insufficiency
- Should not be confused with aplastic crisis, a condition in which erythropoiesis is temporarily suppressed (e.g., due to parvovirus B19 infection in patients with hemolytic anemias)
- Etiology
- Idiopathic in > 50% of cases
- Possibly immune-mediated
- May follow acute hepatitis (hepatitis-associated aplastic anemia)
- Medication side effects: carbamazepine, methimazole, NSAIDs, chloramphenicol, propylthiouracil, sulfa drugs, cytostatic drugs (esp. alkylating agents and antimetabolites)
- Dose-dependent reactions are caused by medications (eg, chemotherapy, immunosuppressives) that are toxic to the bone marrow when drug levels exceed a certain concentration for a certain period. They tend to be predictable in onset.
- Idiosyncratic reactions are often caused by antiseizure medications (eg, carbamazepine, valproic acid), sulfonamides, or nifedipine. They are unpredictable, unrelated to the dose of the drug, and may occur at any point during or after therapy. Although the mechanism is unclear, patients often have genetic mutations in drug-metabolizing enzymes or efflux pumps, which may promote toxicity.
- Toxins: benzene, cleaning solvents, insecticides, toluene
- Ionizing radiation
- Viruses: HBV, EBV, CMV, HIV
- Fanconi anemia
- Hereditary autosomal recessive disorder due to a DNA crosslink repair defect resulting in bone marrow failure
- Skeletal and organ abnormalities: short stature, hypo- and hyperpigmentation, cafe-au-lait spots, microcephaly, developmental delay, thumb and forearm malformations, kidney, GI, heart, eye, and ear abnormalities
- Laboratory tests show pancytopenia and normocytic or macrocytic anemia.
- ∼ 50% of patients with Fanconi anemia will develop acute myeloid leukemia or myelodysplastic syndromes in early adulthood.
- Idiopathic in > 50% of cases
- Pathophysiology
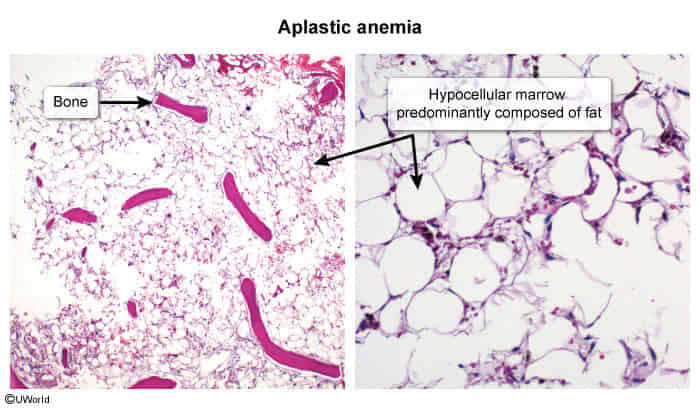
- Multipotent hematopoietic stem cells are destroyed by cytotoxic T cells or direct cytotoxic injury → bone marrow aplasia/hypoplasia → lack of circulating peripheral blood cells
Myelofibrosis vs Aplastic anemia
- Myelofibrosis: splenomegaly
- Evidence of extra medullary hematopoesis
- Aplastic anemia: no
- Explanation: In myeloproliferative disorders like myelofibrosis, niche in marrow is disturbed by slow fibrosis of marrow so stem cells migrate and extra medullary haematopoiesis occurs. But in aplastic anemia (whether primary or secondary to drugs etc) stem cells themselves are destroyed or affected so haematopoiesis not possible anywhere. So we don’t get hepatosplenomegaly and other evidences of extramedullary haematopoiesis.
- Diagnostics
- Laboratory studies, e.g.:
- CBC: pancytopenia (in contrast to aplastic crisis characterized by anemia only), or normocytic or macrocytic anemia
- Reticulocyte count: low
- Erythropoietin level: high
- Bone marrow findings: hypocellular with prominent fat spaces (“empty marrow” appearance)
- Laboratory studies, e.g.: