Definitions
graph TD CAD["Coronary Artery Disease (CAD)"] StableAngina["Chronic Stable Angina"] ACS["Acute Coronary Syndrome (ACS)"] UnstableAngina["Unstable Angina"] NSTEMI["NSTEMI"] STEMI["STEMI"] Variant["Variant (Prinzmetal) Angina"] CAD --> StableAngina CAD --> ACS CAD --> Variant ACS --> UnstableAngina ACS --> NSTEMI ACS --> STEMI
| Feature | Chronic Stable Angina | Unstable Angina (UA) | NSTEMI | STEMI | Vasospastic (Prinzmetal) Angina |
|---|---|---|---|---|---|
| Pathophysiology | Fixed >70% stenosis | Plaque rupture, sub-occlusive thrombus | Plaque rupture, sub-occlusive thrombus | Plaque rupture, occlusive thrombus | Coronary artery spasm |
| Chest Pain | Predictable, on exertion; lasts <20 min | Unpredictable, at rest or crescendo pattern | Prolonged, severe, at rest | Prolonged, severe, crushing, at rest | Episodic, at rest (often nocturnal) |
| Relieved by Rest/NTG | Yes | Often not | No | No | Yes (spontaneously or w/ NTG) |
| ECG Findings | Normal at rest; ST depression on stress | ST depression / T-wave inversion (or normal) | ST depression / T-wave inversion (or normal) | ST Elevation (or new LBBB) | Transient ST Elevation during pain |
| Cardiac Biomarkers | Negative | Negative | Positive | Positive | Negative |
| Key Management | Medical Tx (ASA, β-blocker, Statin), NTG prn | Anticoagulation (Heparin), dual antiplatelet therapy (DAPT) | Anticoagulation, DAPT; often early invasive strategy (PCI) | Emergent Reperfusion (PCI <90min or Fibrinolysis) | CCBs, Nitrates; AVOID non-selective β-blockers |
Coronary artery disease
- Coronary artery disease (CAD): ischemic heart disease due to narrowing or blockage of coronary arteries, most commonly due to atherosclerosis, resulting in a mismatch between myocardial oxygen supply and demand
- Stable CAD: a form of CAD in which patients are either asymptomatic or have stable or low-risk unstable angina; also used for patients with a history of MI whose symptoms are controlled with treatment
Chest pain and angina
Preferred terminology for types of chest pain
- Cardiac chest pain: likely associated with cardiac ischemia based on symptoms (e.g., central, retrosternal, squeezing, exertional).
- Possible cardiac chest pain: may be associated with cardiac ischemia based on symptoms (e.g., stabbing, tearing, ripping, burning).
- Noncardiac chest pain: unlikely associated with cardiac ischemia based on symptoms (e.g., positional, fleeting).
Historical terminology for types of chest pain
The following terms are no longer recommended for use in the 2021 AHA/ACC chest pain guidelines.
- Typical angina fulfills all of the following criteria:
- Retrosternal chest pain of characteristic nature and duration (e.g., transient retrosternal pressure)
- Provoked by exertion or emotional stress
- Relieved by rest and/or nitroglycerin
- Atypical angina: fulfills only two of the aforementioned criteria
- Nonanginal chest pain: fulfills one or none of the aforementioned criteria
Epidemiology
Etiology
Pathophysiology
- Mild Stenosis (<50%) t
- Often termed “non-obstructive” CAD.
- Fractional flow reserve (FFR) is usually >0.95
- Not benign; associated with a higher risk of cardiac events compared to having no CAD.
- Can cause ACS via plaque rupture.
- Intermediate Stenosis (50-70%)
- Considered an anatomical “gray zone” where physiologic significance is uncertain.
- Fractional Flow Reserve (FFR) is the gold standard to determine if the lesion is causing ischemia.
- FFR ≤ 0.80 indicates a hemodynamically significant stenosis that is likely to be causing ischemia and may benefit from revascularization.
- FFR > 0.80 suggests the stenosis is not flow-limiting, and revascularization can often be safely deferred in favor of medical therapy.
- Severe Stenosis (≥70%)
- Considered hemodynamically significant and obstructive.
- High likelihood of causing ischemia and adverse outcomes.
- For the Left Main (LM) coronary artery, a stenosis of ≥50% is considered severe and is a high-risk finding, as it supplies a large portion of the myocardium.
| Feature | Stable Plaque | Unstable (Vulnerable) Plaque |
|---|---|---|
| Fibrous Cap | Thick, strong, intact | Thin, weak, prone to rupture/erosion |
| Lipid Core | Smaller, less necrotic | Larger, highly necrotic, soft |
| Inflammation | Low | High (active macrophages, MMPs) |
| Smooth Muscle | More, synthesizing collagen | Fewer, more apoptosis |
| Primary Problem | Slow development. Allow the development of viable collateral vessels | Rupture/Erosion & Thrombosis |
| Clinical Risk | Stable Angina, Claudication | Acute Coronary Syndromes (MI, UA), Stroke |
| Acute Event Risk | Lower | Higher |
Clinical features
Stable angina
- Symptoms are reproducible/predictable and severity, frequency, and threshold for reproduction of symptoms do not change.
- Symptoms often subside within minutes with rest or after administration of nitroglycerin
- Common triggers include physical/mental stress or exposure to cold
Anginal equivalents
- High-Risk Groups: Women, Elderly, Diabetics (autonomic neuropathy masks pain), Transplant patients.
- Key Symptoms: Dyspnea without pain (most common), epigastric pain (“indigestion”), nausea/vomiting, diaphoresis, syncope. c
- Diagnostic Rule: Any high-risk patient with vague upper abdominal or respiratory symptoms gets an ECG first. Do not treat for GERD before ruling out ACS.
- Classic Trap: Diabetic patient + Nausea/Vomiting/Epigastric pain = Inferior MI until proven otherwise.
Diagnostics
Treatment
Stable Ischemic Heart Disease (SIHD)
- Goal: Prevent future MI/death & control angina.
- Medical Tx (Universal):
- Antiplatelet: Aspirin (or Clopidogrel if allergic).
- Statin: High-intensity (e.g., Atorvastatin) for ALL patients.
- Symptom (Angina) Control:
- 1st Line: Beta-blockers.
- Acute Relief: Sublingual Nitroglycerin (NTG).
- Add-on Tx: Calcium Channel Blockers (CCBs), long-acting nitrates.
- Revascularization (PCI/CABG):
- For refractory symptoms despite max medical Tx or high-risk anatomy (e.g., Left Main, 3-vessel disease).
- CABG > PCI for diabetics and complex multi-vessel disease.
Acute Coronary Syndrome (ACS: UA, NSTEMI, STEMI)
- Immediate Tx (All ACS):
- DAPT: Aspirin + P2Y12 inhibitor (e.g., Clopidogrel, Ticagrelor).
- Anticoagulation: Heparin (UFH or LMWH).
- High-Intensity Statin.
- Nitroglycerin: Sublingual (0.4 mg) q5min x3 for chest pain.
- Indication: BP > 90, not Inferior MI
- Contraindication: Right Ventricular MI (II, III, aVF leads) or Sildenafil use within 24h. c
- Symptom Control: NTG, Morphine, Beta-blockers (if stable).
- STEMI-Specific Tx:
- IMMEDIATE REPERFUSION.
- PCI: Gold standard. Goal: door-to-balloon < 90 min.
- Thrombolysis: If PCI is not available (>120 min away).
- NSTEMI / UA-Specific Tx:
- Risk Stratify (TIMI score).
- High-risk: Early invasive strategy (angiography ± PCI).
- Low-risk: Conservative medical management initially.
Right Ventricular Infarct (Inferior Wall MI)
- Clue: ST elevation in II, III, aVF. Hypotension, Clear lungs, JVD.
- Next Step: Get Right-sided ECG (look for ST elevation in V4R).
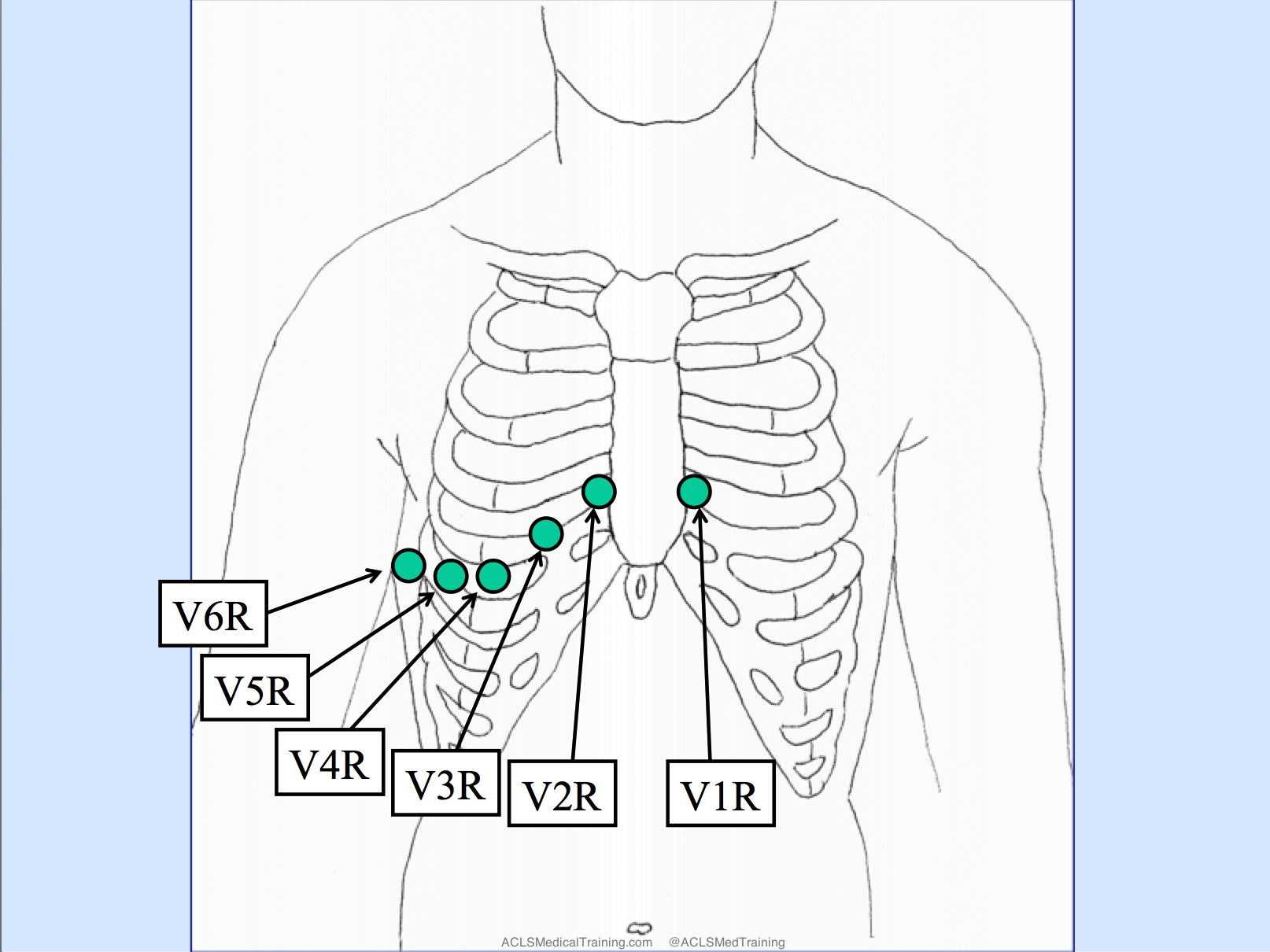
- Management: IV Fluids (maximize preload). Avoid Nitrates/Diuretics (they drop preload).
Subtypes and variants
Vasospastic angina
Previously known as variant or Prinzmetal angina
Description
- Angina caused by transient coronary spasms (usually due to spasms occurring close to areas of coronary stenosis)
- Not affected by exertion (may also occur at rest)
- Typically occurs early in the morning
Etiology
- Cigarette smoking; use of stimulants (e.g., cocaine, amphetamines), alcohol, or triptans
- Stress, hyperventilation, exposure to cold
- Common atherosclerotic risk factors (except smoking) do not apply to vasospastic angina.
Pathogenesis
- Hyperreactivity of coronary smooth muscle due to endothelial dysfunction & autonomic imbalance
- Triggered by excess vagal tone, and they occur most commonly at night when vagal tone is at a peak.
- Both acetylcholine and ergot alkaloids (eg, dihydroergotamine) provoke symptoms and may also aid in diagnosis, as follows:
- Acetylcholine normally stimulates endothelial muscarinic receptors to cause vasodilation via increased release of nitric oxide. However, a deficiency of endothelial nitric oxide in affected patients causes increased vagal tone to instead trigger vasoconstriction and precipitate vasospastic symptoms.
- Ergot alkaloids activate 5-HT2 serotonergic receptors to cause vasoconstriction. Normally, the vasoconstriction is somewhat offset by endothelial release of vasodilatory prostaglandins, but this response is lacking in affected patients due to endothelial dysfunction.
Clinical presentation
- Young age (<50)
- Minimal CAD risk factors (other than smoking)
- Recurrent chest discomfort
- At rest or during sleep
- Spontaneous resolution ≤15 min
Diagnosis
- ECG: ST-segment elevation during episode
- Coronary angiography: no CAD
Treatment
- Smoking cessation
- Avoid beta-blockers (particularly nonselective beta blockers), and other agents that induce vasoconstriction
- Blockade of beta-2 receptors prevents smooth muscle cell relaxation and may cause additional vasoconstriction.
- First-line therapy: calcium channel blockers, e.g., verapamil, diltiazem, or nifedipine