Epidemiology
- Onset of symptoms usually occurs at 3–6 months of age.
- Disease often improves with age.
Etiology
Pathophysiology
The pathogenesis of atopic dermatitis involves immune dysregulation and genetically mediated skin barrier dysfunction (eg, filaggrin mutation). The epidermal dysfunction increases cutaneous exposure to environmental allergens, which induce a Th2-predominant immune response. Key Th2 cytokines that trigger acute inflammation in atopic dermatitis are IL-4 and IL-13, and mechanisms include the following:
- Stimulation of plasma cell IgE production, which facilitates allergen sensitization and inflammation
- Suppressed expression of epidermal barrier components, which enhances Staphylococcus aureus colonization and inflammation
- Inhibition of Th1-type immune response and antimicrobial peptide production, which facilitate secondary microbial infections that complicate atopic dermatitis
Clinical features
Tip
The symptoms of atopic dermatitis are variable and often change in the course of a lifetime. Pruritus and dry skin are usually the main symptoms. Most patients have a history of other atopic disorders
- Main symptoms: intense pruritus and dry skin
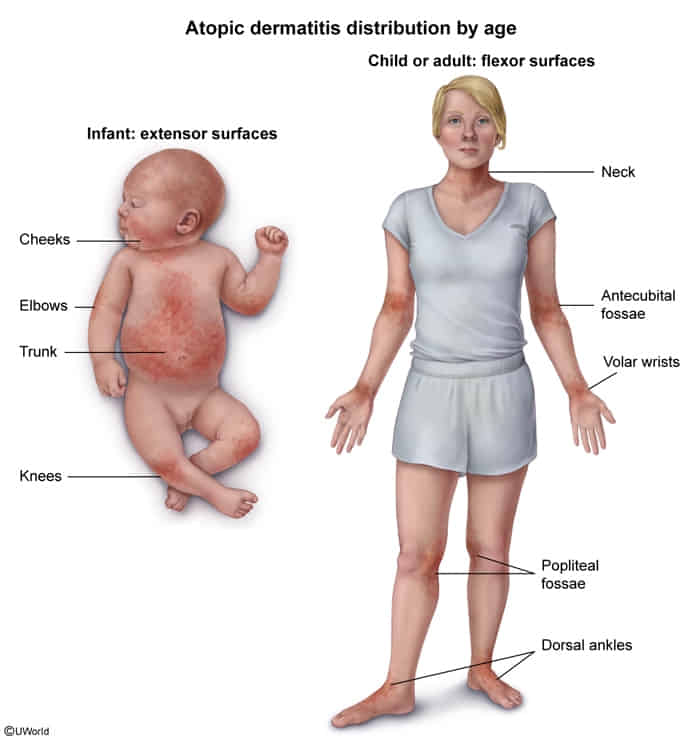
- Infantile AD (age < 2 years)
- Eczema involving the face, head, and extensor surfaces of the extremities that usually spares the diaper area
- May present initially with features similar to seborrheic dermatitis, e.g., cradle cap
- Dennie-Morgan fold: increased folds below the eye
- as a result of eyelid dermatitis

- as a result of eyelid dermatitis
- Occasionally, lesions appear on the trunk.
- Childhood AD (age 2–12 years)
- Eczema: flexural creases (antecubital fossa and popliteal fossa), skin folds, extensor surface of hands
- Lesions usually become lichenified (thickening of the skin with accentuated skin markings).

- Adult/adolescent AD (age > 12 years)
- Lichenified lesions and pruritus of flexor surfaces of the extremities
- Antecubital fossae are frequently involved.
- Adult AD may also present as nummular eczema.
- Associated skin findings in AD
- Atopic triad: a triad of asthma, allergic rhinitis, and atopic dermatitis that is linked to allergen-triggered IgE-mast cell activation
- Food allergies
- Keratosis pilaris: keratinized hair follicles (rough bumps) typically distributed over extensor arms and thighs
- Hertoghe sign: thinning or loss of the outer third of the eyebrows
Diagnostics
- Atopy
- Personal and/or family history
- Immunoglobulin E reactivity (↑ serum IgE)
- Comorbid atopic diseases (i.e., asthma, allergic rhinitis, allergic conjunctivitis, and food allergies)
Treatment
- Topical steroids (preferred)
- Topical calcineurin inhibitors