Epidemiology
Etiology
Central diabetes insipidus (CDI)
- Most common form: caused by insufficient or absent hypothalamic synthesis or posterior pituitary secretion of ADH
- Primary (∼ ⅓ of cases)
- Secondary (∼ ⅔ of cases)
- Brain tumors (especially craniopharyngioma)
- Neurosurgery
- Traumatic brain injury, pituitary bleeding, subarachnoid hemorrhage
- Pituitary ischemia (e.g., Sheehan syndrome, ischemic stroke)
Nephrogenic diabetes insipidus (NDI)
- Rare: caused by defective ADH receptors in the distal tubules and collecting ducts
- Hereditary (mutation in ADH receptor): very rare
- Acquired: typically reversible if the underlying cause is resolved
- Adverse effect of medications (lithium, demeclocycline)
- Hypokalemia, hypercalcemia
Pathophysiology
Tip
Note that in central DI, ADH levels are decreased, while in nephrogenic DI, they are normal or increased to compensate for the high urine output.
Clinical features
- Polyuria with dilute urine
- Nocturia → restless sleep, daytime sleepiness
- Polydipsia (excessive thirst)
- In cases of low water intake → severe dehydration (altered mental status, lethargy, seizures, coma) and hypotension
- Symptoms may worsen during pregnancy.
Tip
In the absence of nocturia, diabetes insipidus is very unlikely.
Diagnostics
Serum sodium and plasma osmolality
- ↓ Na+ and/or ↓ plasma osmolality: primary polydipsia likely
- Normal values: diagnosis unclear; obtain subsequent studies to differentiate between polyuria-polydipsia syndromes.
- ↑ Na+ and/ or ↑ plasma osmolality: Diabetes insipidus likely; obtain subsequent studies to differentiate between CDI and NDI.
Water deprivation test (indirect assessment of ADH activity)
Urine concentrating capacity is assessed during a period of dehydration; desmopressin is then administered to assess response to a synthetic ADH analogue.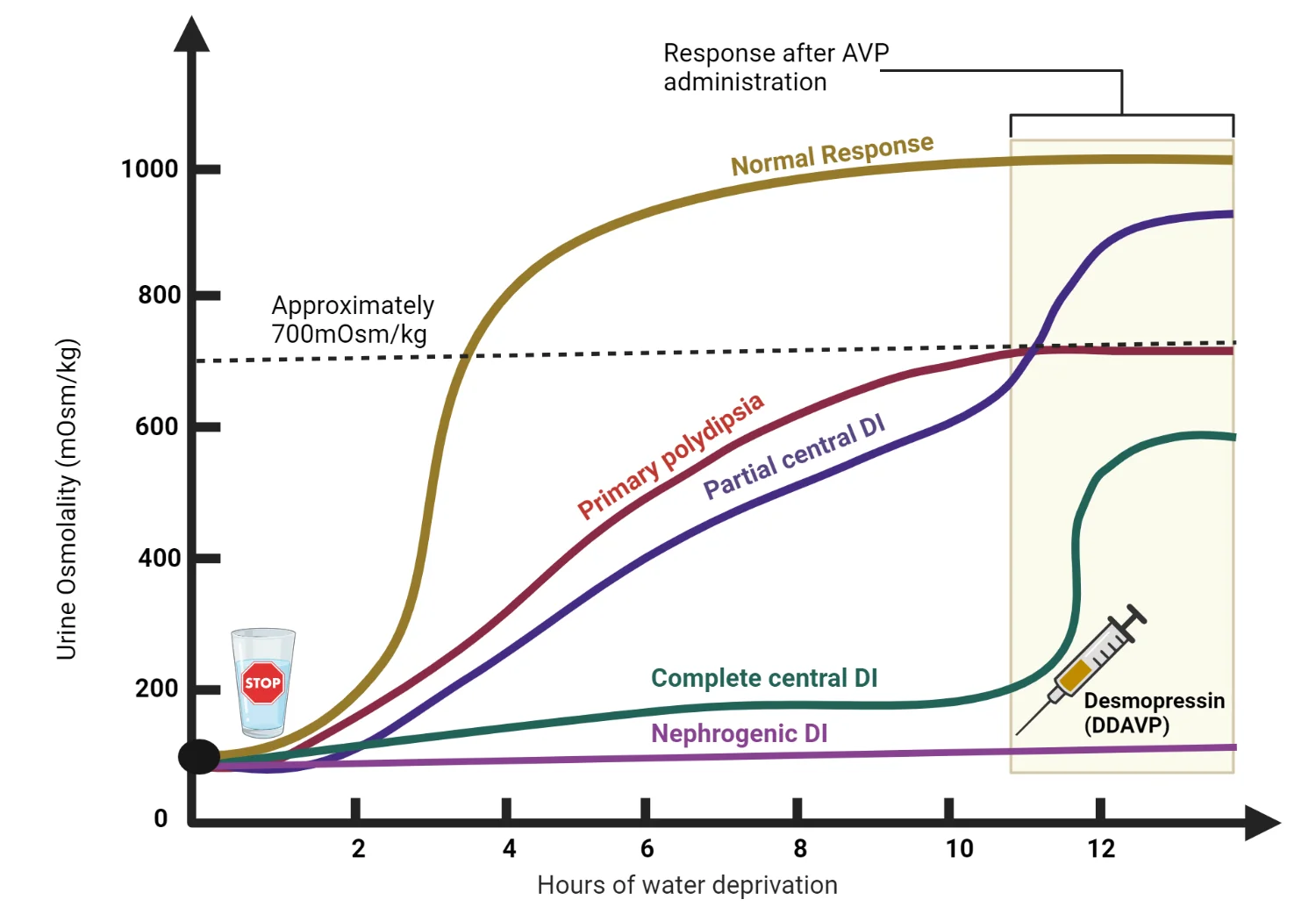
- Interpretation after period of water deprivation
- Urine osmolality increases to > 800 mOsm/kg: Primary polydipsia is confirmed.
- Urine osmolality remains ≤ 800 mOsm/kg: Administer desmopressin (a synthetic ADH analogue).
- Interpretation after desmopressin administration
- Urine osmolality (300–800 mOsm/kg) and:
- Significant increase (≥ 10%) after desmopressin: partial CDI
- No or minimal increase (< 10%) after desmopressin: primary polydipsia
- Urine osmolality (< 300 mOsm/kg) and:
- Significant increase (> 50%) after desmopressin: complete CDI (indicating intact renal ADH receptors)
- No or moderate increase (< 50%) after desmopressin: NDI (indicating defective renal ADH receptors)
- Urine osmolality (300–800 mOsm/kg) and:
Differential diagnostics
Primary polydipsia (psychogenic polydipsia)
- Mechanism
- Compulsive water intake
- Etiology
- Psychiatric diseases (e.g., schizophrenia, obsessive-compulsive disorder)
- Lesions in the hypothalamic thirst center
- Features
- Hyponatremia
- Low plasma osmolarity, very low urine osmolarity
- Water deprivation: plasma and urine osmolarity increase to normal level
Treatment
Encourage adequate fluid intake and a low-sodium, low-protein diet.
Central diabetes insipidus
- Desmopressin (preferred): synthetic ADH analogue without vasoconstrictive effects
- Intranasal administration is preferred.
- Chlorpropamide
Nephrogenic diabetes insipidus
- Treat the underlying cause, if applicable, e.g.:
- Discontinue the causative agent (e.g., lithium, demeclocycline).
- Thiazide diuretics
- Lead to sodium depletion, which increases sodium and water reabsorption in the proximal tubules
- As a result, less water reaches the distal collecting tubules and urine volume decreases.
- NSAIDs (e.g., indomethacin)
- Inhibit renal prostaglandins that act as ADH antagonists
- Amiloride