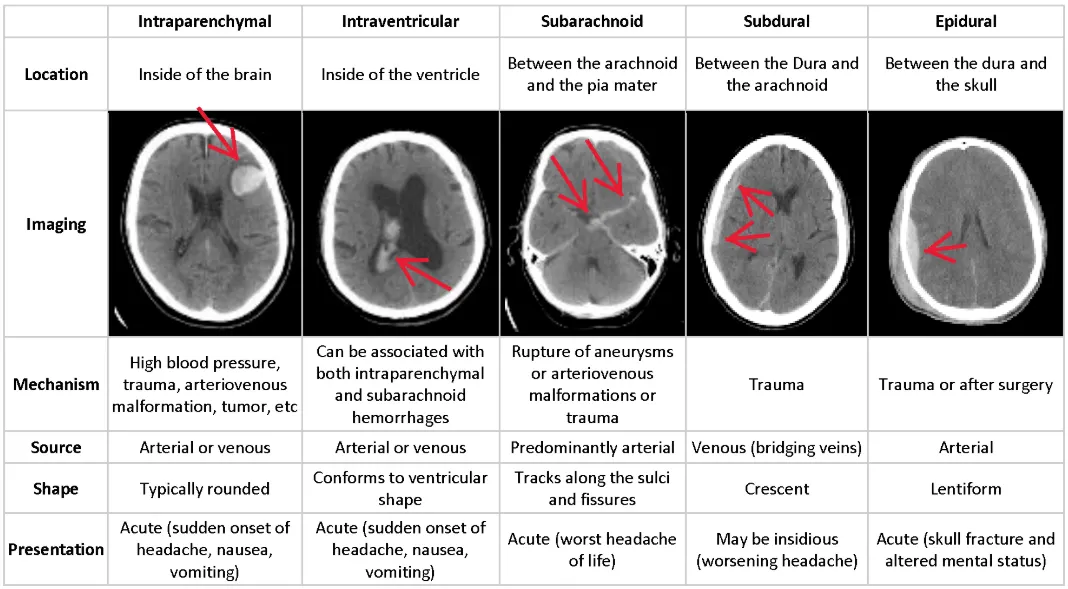
| Type | Vessel / Cause | Key Associations | CT Appearance |
|---|---|---|---|
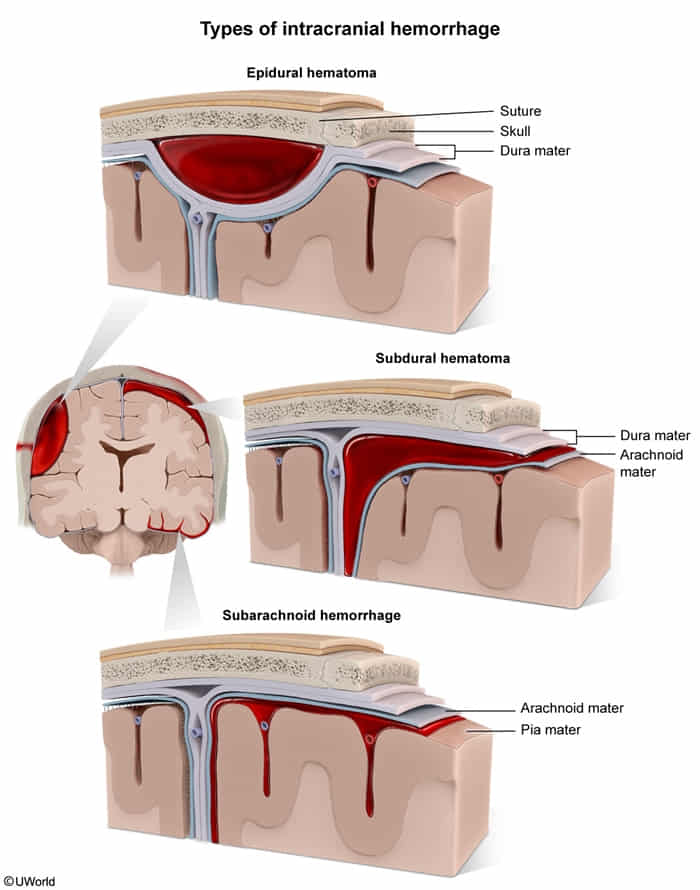
| Epidural | Middle Meningeal Artery | Pterion fracture, Lucid interval | Lens-shaped (Biconvex) Stops at sutures |
| Subdural | Bridging Veins | Elderly, Alcoholics, Shaken Baby | Crescent-shaped Crosses sutures |
| Subarachnoid | Berry Aneurysm / AVM | ”Thunderclap” headache, Meningeal signs | Blood in Sulci LP: Xanthochromia |
| Intraparenchymal | Charcot-Bouchard (HTN) | HTN, Amyloid angiopathy, Basal Ganglia | Focal hyperdensity within brain |
| Intraventricular | Germinal Matrix | Premature infants (<32 wks) | Blood inside Ventricles |
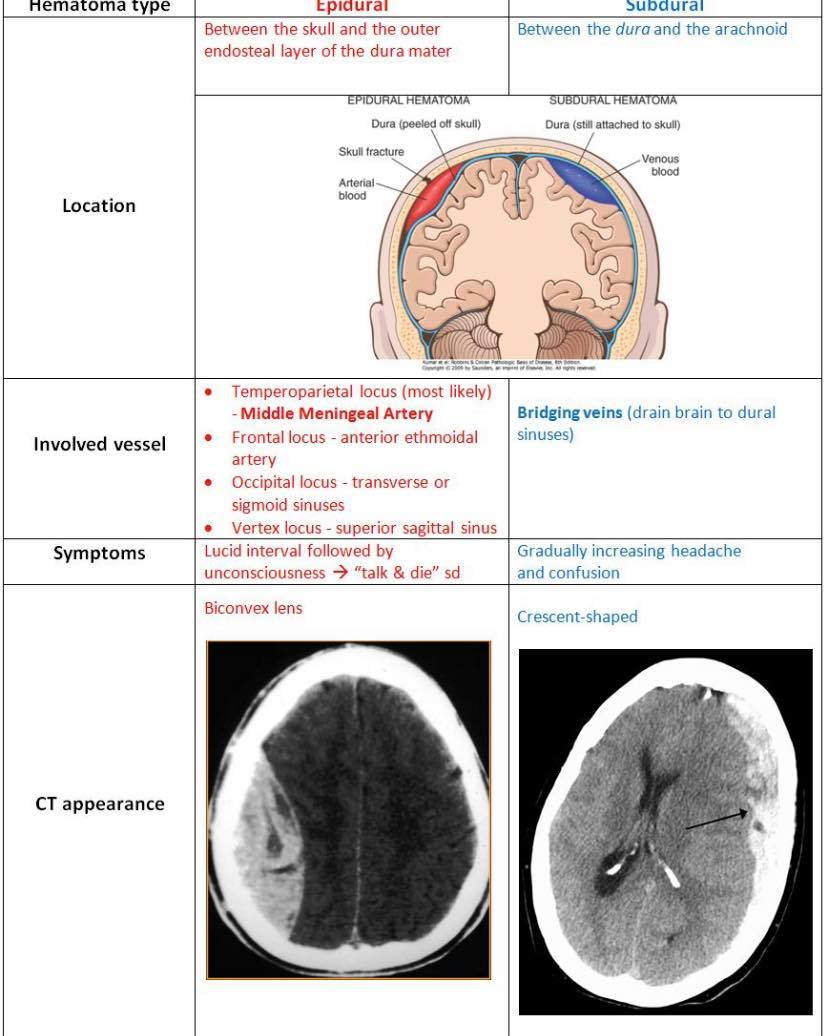
Epidural hematoma
Subarachnoid hemorrhage
Etiology
- Elderly individuals experience age-related cerebral atrophy. This brain shrinkage puts increased tension on the bridging veins, making them highly susceptible to tearing from shearing forces, even with relatively minor head trauma (like a fall).
- Traumatic SAH: traumatic brain injury
- Nontraumatic (spontaneous) SAH
- Ruptured intracranial aneurysms
- Most commonly occur in the circle of Willis
- Berry aneurysms account for approx. 80% of cases of nontraumatic SAH.
- Also known as Saccular aneurysm because of the shape
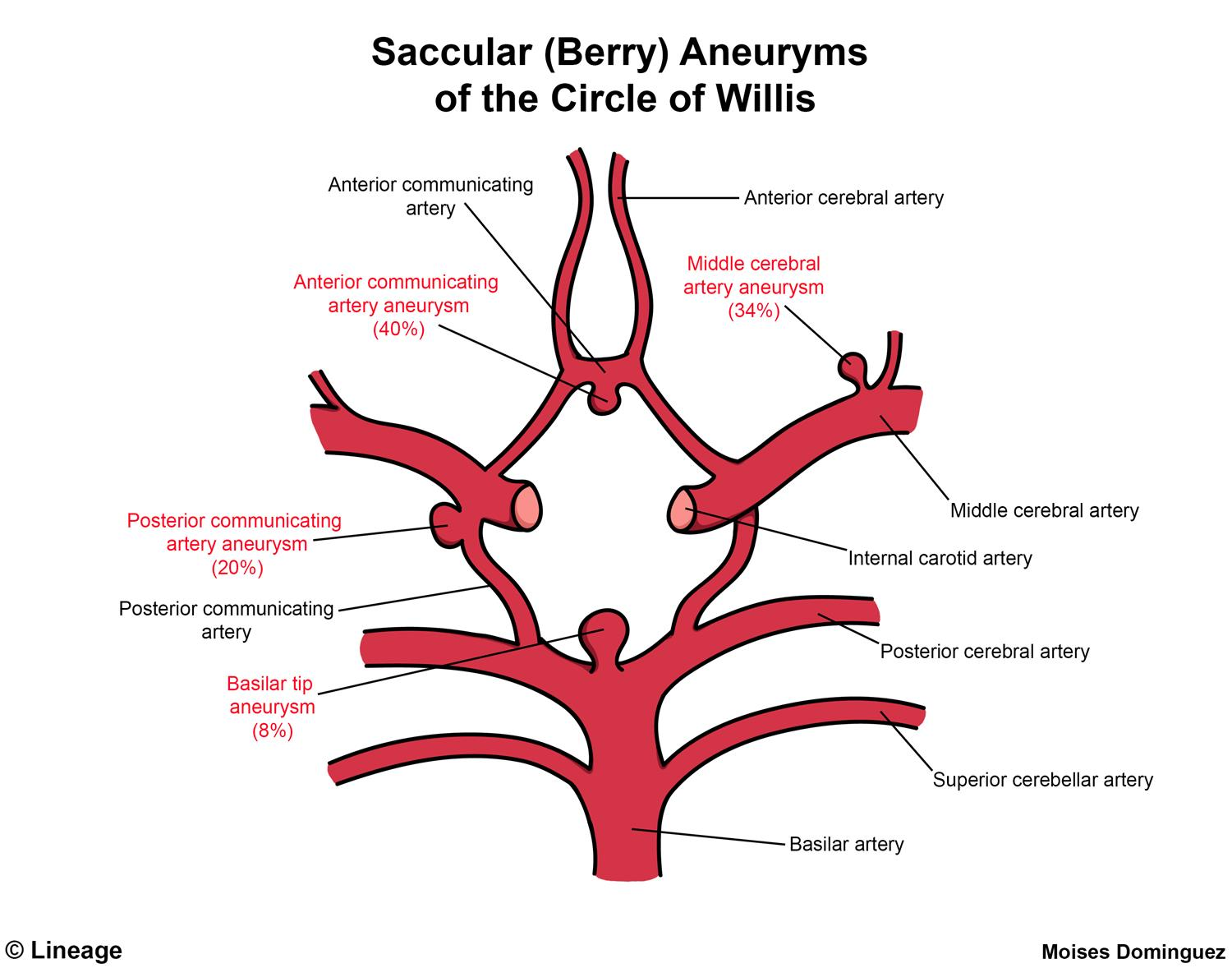
- Round, saccular shape
- Most common type of cerebral aneurysm
- Typically occur at vessel junctions in the circle of Willis, most commonly between the anterior communicating artery and anterior cerebral artery
- Account for ∼ 80% of cases of nontraumatic subarachnoid hemorrhage
- Also known as Saccular aneurysm because of the shape
- Ruptured arteriovenous malformations (AVM)
- Ruptured intracranial aneurysms
Charcot-Bouchard aneurysms vs Saccular (berry) aneurysms
Feature Charcot-Bouchard Saccular (Berry) Etiology Chronic HTN Congenital weakness + Hemodynamics Pathology Lipohyalinosis of microvessels Lacking Internal Elastic Lamina & Media Location Deep Brain (Basal Ganglia, Thalamus) Circle of Willis Bifurcations (ACom > PCom) Vessels Lenticulostriate arteries Medium-sized arteries Rupture Intraparenchymal Hemorrhage Subarachnoid Hemorrhage Symptoms Focal deficits (Hemiparesis) “Thunderclap” Headache, Meningismus Associations Lacunar strokes ADPKD, Ehlers-Danlos, Marfan
-aneurysms/../../../appendix/Pasted-image-20250304102040.png)
Link to original
- Saccular: This term means “resembling a sac.” Saccular aneurysms are outpouchings or bulges on one side of a blood vessel wall.
- Berry: The “berry” description refers to the characteristic round shape of these aneurysms. They look like a berry connected to the main artery.
Clinical Features
- Gradual/Insidious Onset: Neurologic decline over hours to days.
- Sx: Headache, somnolence, confusion, light-headedness, focal neurologic deficits (e.g., focal weakness).
- Chronic SDH (weeks to months old): Can present with subtle cognitive impairment, dementia-like symptoms, and gait disturbances, particularly in the elderly.
Diagnosis
CT head without contrast
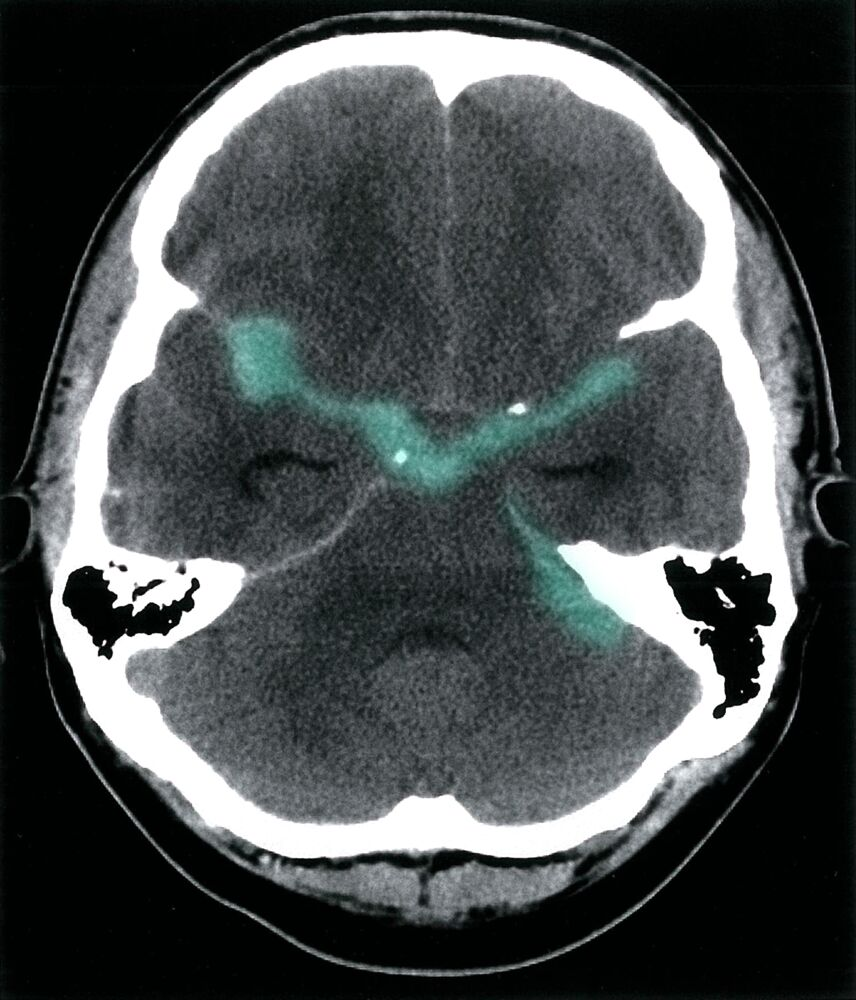
- Defining feature: blood in subarachnoid space (hyperdense) with variable extension and location
Treatment
Initial management
- Prevention of rebleeding
- Anticoagulant reversal
- Management of blood pressure and cerebral perfusion pressure
- Target SBP < 160 mm Hg
- Other neuroprotective measures
- Start ICP management (e.g., elevate head 30°, IV mannitol, short-term controlled hyperventilation).
Treatment of aneurysmal SAH
- Intracranial aneurysm repair
- Endovascular coiling
- Microsurgical clipping
- Prevention of vasospasm and delayed cerebral ischemia
- Administer oral nimodipine
- Only administer nimodipine orally or via enteral tube; Parenteral administration is associated with significant adverse effects (e.g., severe hypotension and cardiac arrest).
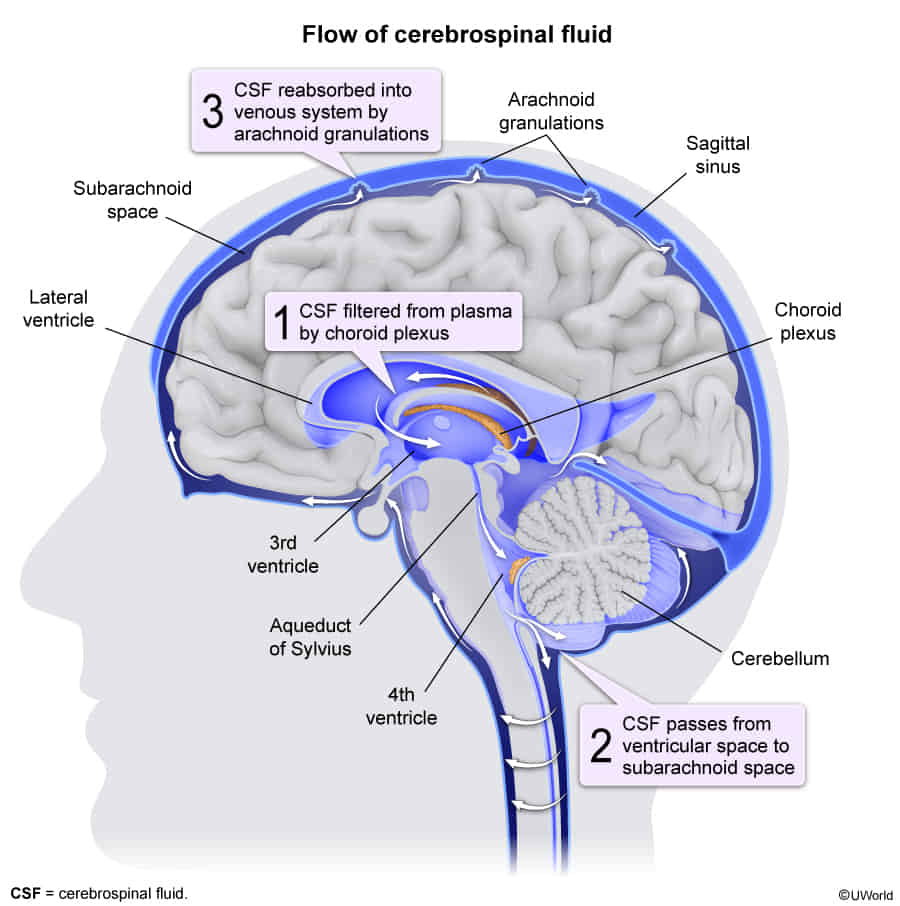
- Treatment of hydrocephalus: may include an external ventricular drain (EVD), lumbar drainage, or permanent ventriculoperitoneal shunt
- Administer oral nimodipine
Warning
Generally avoid nitrates for blood pressure control in brain injury, as they may elevate ICP. Consider alternative agents (e.g., titratable nicardipine or labetalol).
Complications
Vasospasm
- Occurs in approx. 30% of patients with SAH
- Pathophysiology
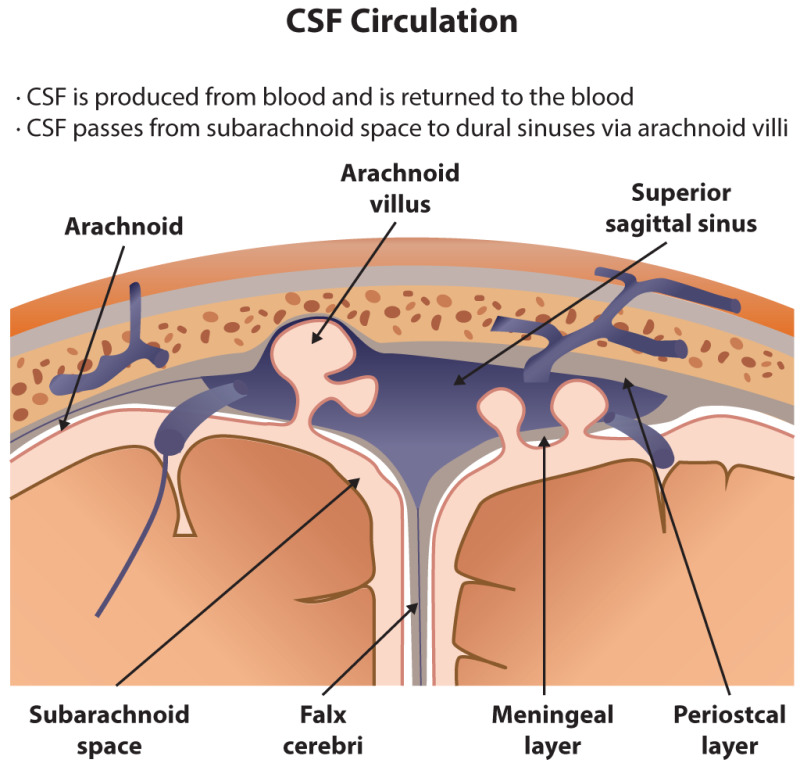
- Impaired CSF reabsorption from the arachnoid villi → nonobstructive (communicating) hydrocephalus → ↑ intracranial pressure → ↓ cerebral perfusion pressure → ischemia
- Release of clotting factors and vasoactive substances → diffuse vasospasm of cerebral vessels → ischemia
- Impaired CSF reabsorption from the arachnoid villi → nonobstructive (communicating) hydrocephalus → ↑ intracranial pressure → ↓ cerebral perfusion pressure → ischemia
- Can lead to ischemic stroke
- Most common in patients with nontraumatic SAH due to a ruptured aneurysm
- Usually occurs between 3–10 days after SAH
- Prevention & Treatment
- Nimodipine (Calcium Channel Blocker): t
- Standard of Care: Started on admission (Day 1) for all SAH patients.
- Mechanism: It blocks this calcium influx into the neurons, preventing cellular death. Prevents ischemic neurological deficits and improves mortality (neuroprotection).
- Note: It does not necessarily prevent the angiographic vasospasm itself, but prevents the cellular injury associated with it.
- Hemodynamic Augmentation (formerly “Triple H”):
- Current Goal: Maintain Euvolemia and Induced Hypertension (using vasopressors like phenylephrine or norepinephrine).
- Rationale: ↑ MAP pushes blood through the narrowed vessels to maintain Cerebral Perfusion Pressure (CPP).
- Refractory Cases:
- Intra-arterial vasodilators (e.g., verapamil, nicardipine).
- Balloon angioplasty (mechanical dilation).
- Nimodipine (Calcium Channel Blocker): t
-aneurysms/../../../appendix/Pasted-image-20240526113641.png)