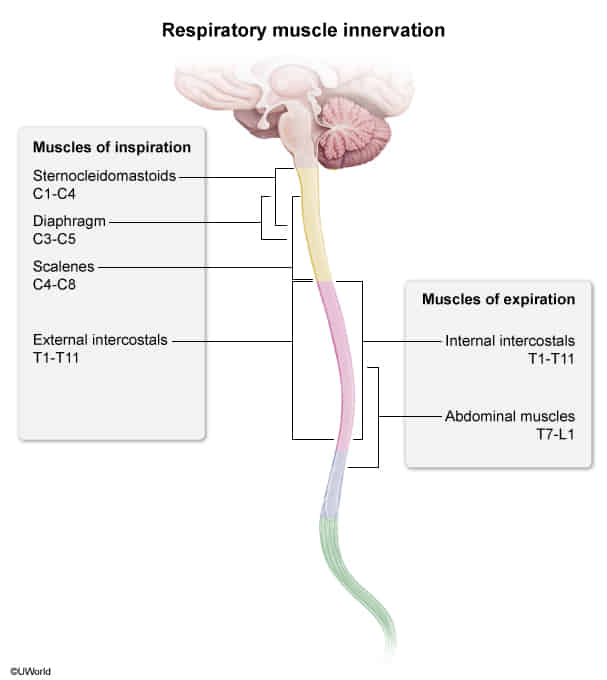
Respiratory muscles
Gas exchange
Types of gas exchange
- Perfusion-limited gas exchange: Gas exchange is limited by the rate of blood flow through the pulmonary capillaries.
- Gases (e.g., O2, CO2, N2O) can diffuse freely across the blood-air barrier.
- The concentration of gases in the plasma will become equal to the concentration in the alveoli before the blood reaches the end of the capillary.
- An increase in blood flow causes an increase in gas exchange .
- Occurrence: under normal conditions (i.e., at rest)
- Diffusion-limited gas exchange: Gas exchange is limited by the diffusion rate of the gas (e.g., O2, CO) across the blood-air barrier.
- The gas concentration in the plasma will not be in equilibrium at the end of the capillary.
- Occurrence
- Strenuous exercise
- In certain pathological conditions that affect the blood-air barrier (e.g., emphysema, lung fibrosis)
Tip
Under normal physiological conditions, O2 transport is generally perfusion-limited, while it can become diffusion-limited in pathological states or during intense exercise.
Anatomy
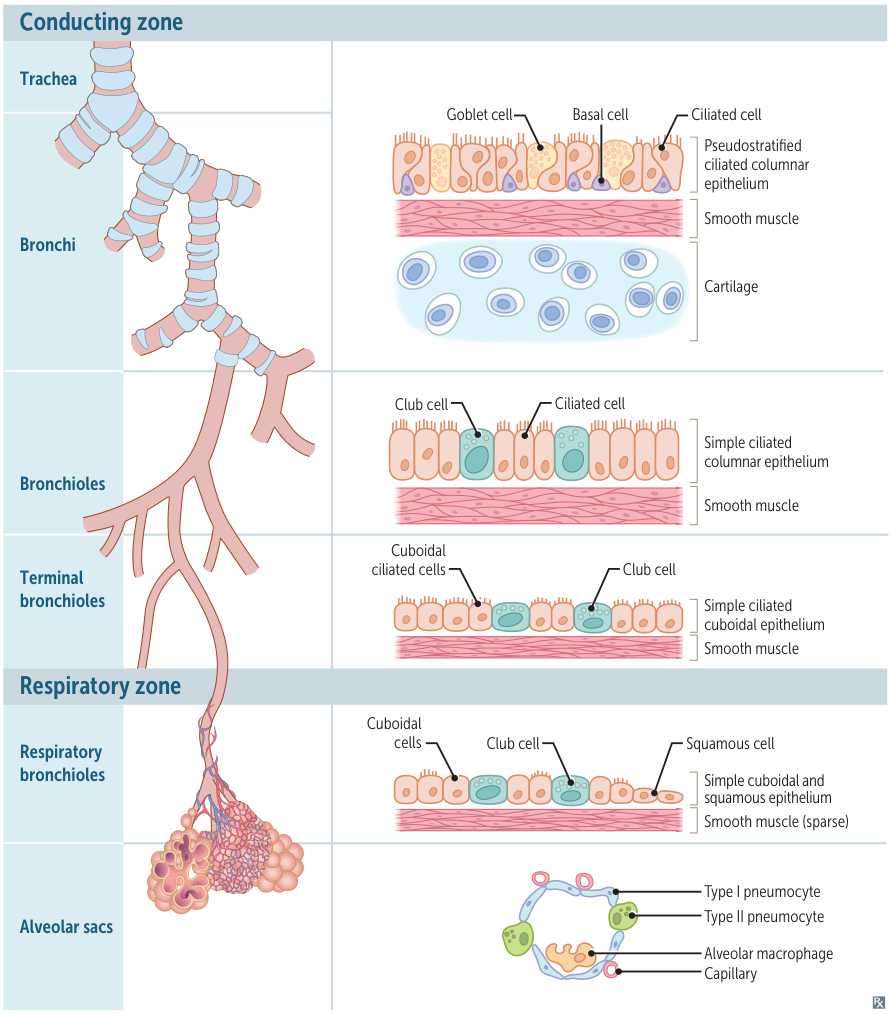 The overall trend in the respiratory tract is for the epithelium to become progressively thinner as it approaches the alveoli (where it’s extremely thin simple squamous epithelium) to facilitate gas diffusion.
The overall trend in the respiratory tract is for the epithelium to become progressively thinner as it approaches the alveoli (where it’s extremely thin simple squamous epithelium) to facilitate gas diffusion.
- Bronchi: all
- Bronchioles
- No cartilage
- Pseudostratified epithelium → Simple epithelium
- – Globlet cells and basal cells
- Globlet cells produce thick mucus, which could cause obstruction in thinner bronchioles. So it’s not needed.
- + Club cells
- Club cells secrete lipoproteins (components of pulmonary surfactant) that reduce surface tension within the small airways. This is crucial to prevent the narrow bronchioles from collapsing, especially during exhalation. Larger airways are held open by cartilage and don’t face the same collapse risk.
- Maintain the integrity of the respiratory epithelium by secreting specialized immunomodulatory proteins, glycoproteins, and lipids.
- Cytochrome P450-dependent degradation of toxins
- Act as a reserve for ciliated cells to restore bronchiolar epithelium (stem cell properties)
- Nonciliated, secretory, cuboidal cells located in the terminal and the respiratory bronchioles of the lung
- – Globlet cells and basal cells
- Terminal bronchioles
- Columnar ciliated cells → Cuboidal ciliated cells
- Respiratory bronchioles
- + Squamous cells
- Alveolar sacs
- All gone
Pneumocytes
- Type I pneumocytes: thin squamous cells that line the alveoli that allow for transcellular gas exchange
- Comprise 95% of the total alveolar area
- Connected to each other by tight junctions
- Form the blood-air barrier, together with the endothelial cells of the capillaries and the basement membrane between the two cells.
- Type II pneumocytes: cuboidal alveolar cells
- Comprise 5% of the total alveolar area, but 60% of total number of cells
- Surfactant formation: Type II pneumocytes contain lamellar bodies, which secrete surfactant (surface-activating lipoprotein complex).
- Surfactant is mainly composed of the phospholipids dipalmitoylphosphatidylcholine (DPPC or lecithin) and phosphatidylglycerol.
- It reduces alveolar surface tension and thereby prevents the alveoli from collapsing.
- Imagine a bubble. The film of the bubble has surface tension, which tends to make the bubble as small as possible. Now, imagine adding a special substance (like surfactant) to the bubble’s film. This substance has one end that likes water and one end that doesn’t. The water-liking ends stick into the film, while the other ends stick out. This disrupts the pull between the water molecules in the film, reducing the surface tension and making it easier for the bubble (alveolus) to stay inflated.
- Lung regeneration and repair: Type II pneumocytes can proliferate to replace type I or type II pneumocytes following lung damage.
Respiratory adaptation
Respiratory adaptation to exercise
- ↑ O2 consumption and ↑ CO2 production lead to ↑ depth and rate of ventilation (hyperventilation).
- ↑ Venous CO2 and ↓ venous O2
- PaCO2 and PaO2 remain normal despite hyperventilation.
- ↑ HR and ↑ SV → ↑ cardiac output → ↑ pulmonary blood flow
- ↓ Arterial pH (due to lactic acidosis)
- Rightward shift of the oxygen dissociation curve
- Oxygen diffusion becomes diffusion-limited (in resting state it is perfusion-limited).
- ↑ V/Q ratio (from base to apex) → V/Q ratio is more evenly distributed throughout the lung during exercise than at rest
Respiratory adaptation to high altitude
Decreased atmospheric oxygen (PiO2) at high altitudes triggers various adaptation mechanisms in the respiratory system. Insufficient adaptation to the high altitude results in altitude sickness.
- ↓ PaO2 → ↑ ventilation rate (stimulated by hypoxemia) → ↓ PaCO2 and ↑ arterial pH (respiratory alkalosis)
- ↑ Renal HCO3- excretion (to compensate for respiratory alkalosis)
- ↑ Pulmonary vascular resistance (Euler-Liljestrand reflex): chronic hypoxia → pulmonary vasoconstriction → pulmonary hypertension → right ventricular hypertrophy
- ↑ Hb and hematocrit (due to chronic hypoxia triggering ↑ erythropoietin levels)
- ↑ 2,3-BPG concentration → ↓ Hb affinity to O2 → rightward shift of the oxygen dissociation curve
- ↑ Number of mitochondria in cells