Renal tubular acidosis (RTA)
- In RTA, there is a normal anion gap metabolic acidosis in patients with normal or almost normal renal function.
- Basically all present with low pH and hypokalemia (except type 4)
- Think H+ and K+ antagonize each other during excretion (due to Na+/K+ vs Na+/H+), increased excretion of one leads to decreased excretion of the other.
- Renal tubular acidosis is caused by defects in the tubular transport of HCO3- and/or H+.
- Most forms of RTA are asymptomatic; rarely, life-threatening electrolyte imbalances may occur.
Remember these alphabetically
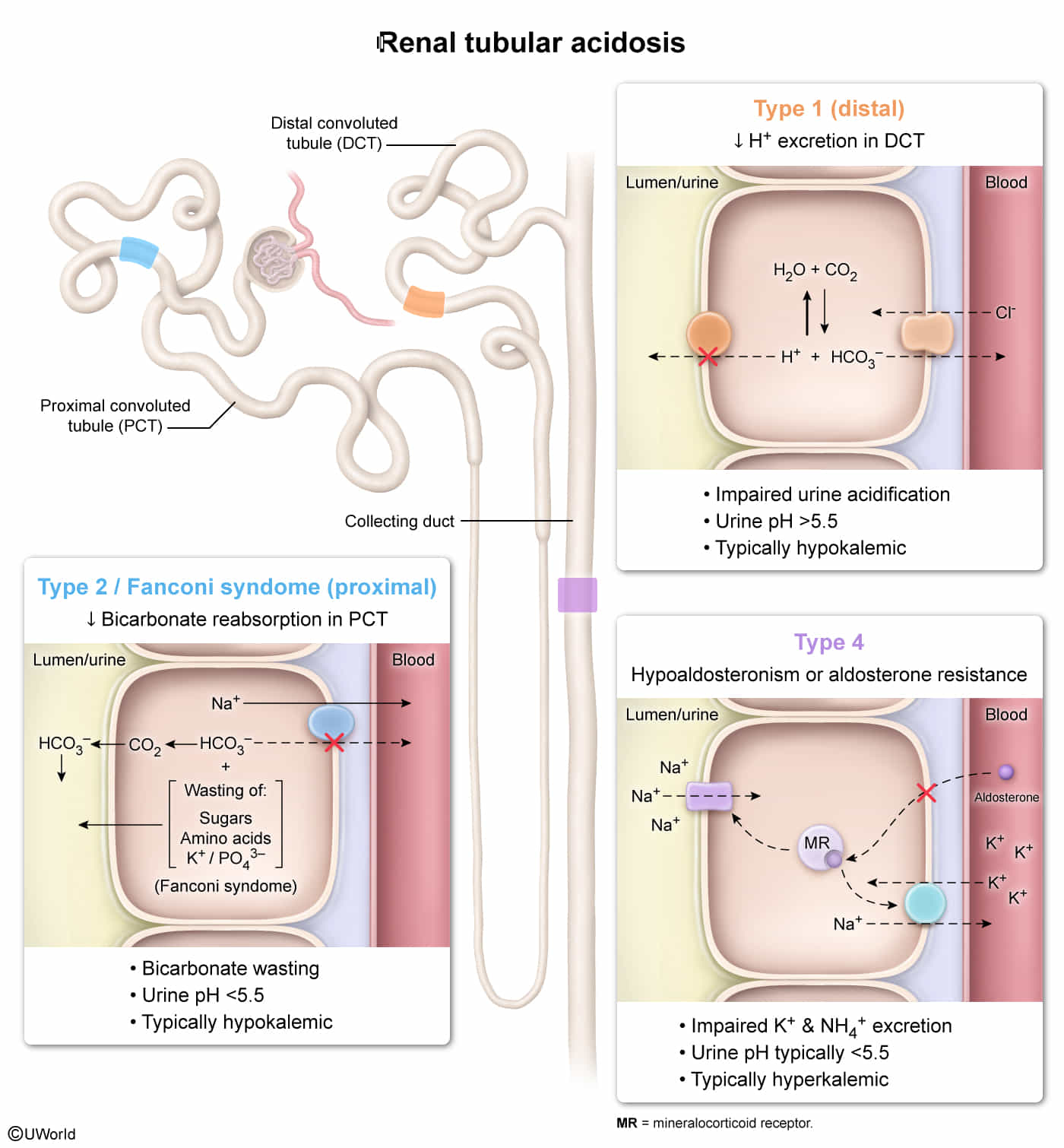
Proximal renal tubular acidosis (type 2)
- Isolated proximal RTA: The proximal convoluted tubule cells are unable to reabsorb HCO3-.
- Fanconi syndrome: Impaired reabsorption of HCO3- and other compounds (e.g., potassium, glucose, phosphate, and amino acid reabsorption) in the PCT
Distal renal tubular acidosis (type 1)
- The α-intercalated cells of the distal tubule are unable to secrete H+.
Mixed RTA (type 3)
- Type 1 RTA with HCO3- wasting
Hyperkalemic renal tubular acidosis (type 4)
- Aldosterone deficiency and/or resistance in the collecting duct and distal convoluted tubule cause hyperkalemia, which inhibits ammonia synthesis in the proximal convoluted tubule and decreases urinary ammonium excretion.