Etiology
- Infection of the endocardium, most commonly affecting heart valves.
- Pathogenesis: Endothelial damage → sterile platelet-fibrin thrombus (nonbacterial thrombotic endocarditis) → transient bacteremia seeds the thrombus → vegetation formation.
Pathogens
- ** S. aureus **: Most common cause overall, especially in IV drug users (IVDU), healthcare-associated infections, and acute, aggressive presentations.
- ** Viridans group streptococci ** (S. sanguinis): Associated with poor dentition and recent dental procedures; typically causes subacute IE on previously damaged valves.
- ** S. bovis (S. gallolyticus) **: Strongly associated with colon cancer; a workup for colonic malignancy is required if isolated.
- Enterococci (E. faecalis): Common after GU/GI procedures and in nosocomial settings.
- Coagulase-negative staphylococci (S. epidermidis): Associated with prosthetic valves, especially within the first year of placement.
- HACEK organisms: Haemophilus, Aggregatibacter, Cardiobacterium, Eikenella, Kingella. Part of normal oral flora, associated with culture-negative endocarditis.
- Fungi (Candida, Aspergillus): Seen in immunocompromised patients, IVDU, and after prolonged antibiotic therapy.
Risk factors for infective endocarditis
- Cardiac conditions
- Acquired valvular disease (e.g., Mitral valve prolapse (most common), rheumatic fever, aortic stenosis, degenerative valvular disease)
- Prosthetic heart valves
- Congenital heart defects (e.g., VSD, bicuspid aortic valve)
- Noncardiac risk factors
- Poor dental status
- Dental procedures
- Nonsterile venous injections (e.g., in IV drug use)
- Intravascular devices
- Surgery
Pathophysiology
- Pathogenesis
- Damaged valvular endothelium → exposure of the subendothelial layer → adherence of platelets and fibrin → sterile vegetation (microthrombus)
- Localized infection or contamination → bacteremia → bacterial colonization of vegetation → formation of fibrin clots encasing the vegetation → valve destruction with loss of function (valve regurgitation)
- Clinical consequences
- Bacterial vegetation → bacterial thromboemboli → vessel occlusion → infarctions
- Emboli can lead to metastatic infections of other organs.
Classifications
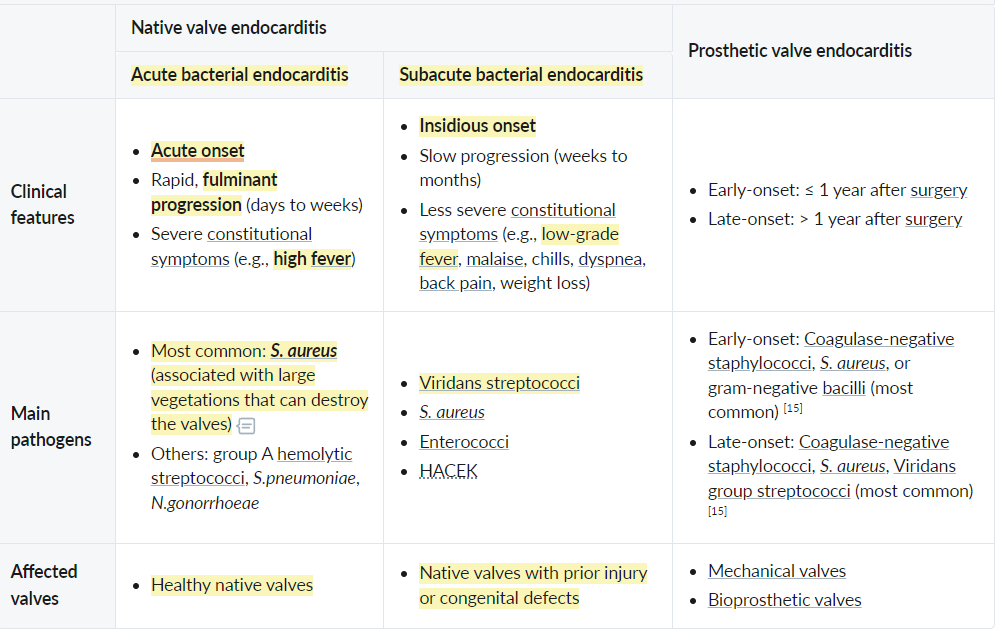 Coagulase-negative staphylococci (CoNS): Staphylococcus epidermidis, Staphylococcus saprophyticus
Coagulase-negative staphylococci (CoNS): Staphylococcus epidermidis, Staphylococcus saprophyticus
Clinical features
Cardiac manifestations
- Development of a new heart murmur or change in a preexisting murmur
- Tricuspid valve regurgitation
- Holosystolic murmur that is loudest at the left sternal border
- Seen in persons who inject drugs, immunocompromised individuals, patients with congenital heart disease, and patients with instrumentation in the right heart (e.g., central venous catheters)
- Aortic valve regurgitation: early diastolic murmur that is loudest at the left 3rd and 4thintercostal spaces and along the left sternal border
- Mitral valve regurgitation: holosystolic murmur that is loudest at the heart’s apex and radiates to the left axilla
- Tricuspid valve regurgitation
Extracardiac manifestations of IE
- Pulmonary manifestations: caused by septic emboli resulting from tricuspid valve involvement
- Signs of pulmonary embolism (e.g., dyspnea)
- Signs of pulmonary infection, e.g., multifocal pneumonia, lung abscess, and/or empyema.
 vs
vs 