Formerly called type 2 HIT
Epidemiology
Etiology
Tip
Heparin treatment, especially with unfractionated heparin (UFH), often causes thrombocytopenia. For this reason, a baseline check and regular monitoring of platelet counts are required.
Pathophysiology
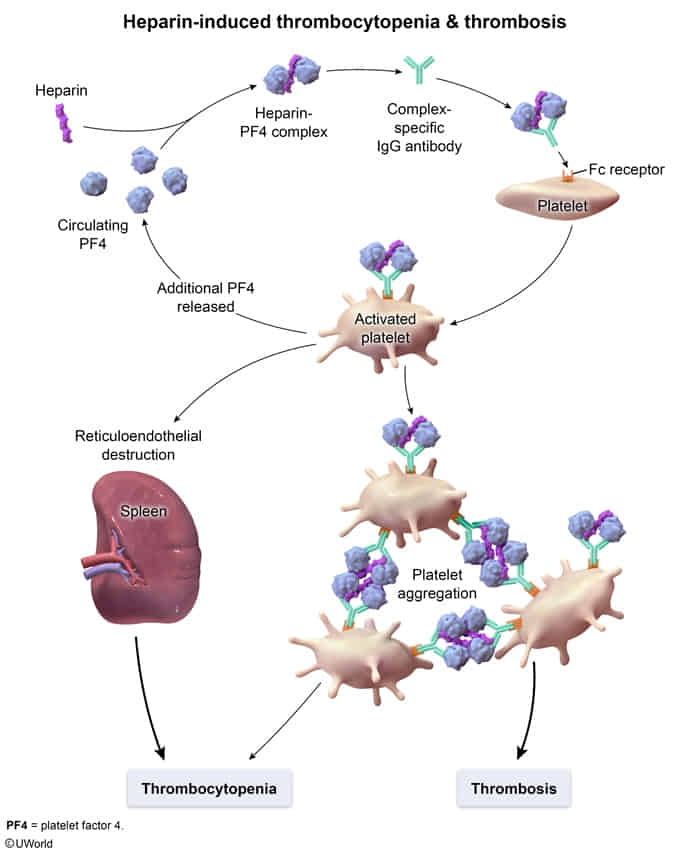
- Heparin and platelet factor 4 (PF4) form a complex → production of IgG antibodies against the heparin/PF4 complex → IgG antibody-heparin/PF4 immunocomplex binds on platelet surface → platelet activation and aggregation → consumption of platelets (thrombocytopenia) and arterial/venous thrombosis
- Thrombocytopenia also occurs due to phagocytosis of IgG antibody-heparin/PF4 immunocomplex-bound platelets by macrophages in the spleen, liver, and bone marrow.
Clinical features
- HIT is primarily a prothrombotic disorder, with venous and/or arterial thrombosis developing in 25–50% of affected patients.
- Venous thrombosis occurs most frequently; manifestations include:
- Calf swelling and pain from lower extremity DVT
- Arterial thrombosis occurs less commonly
- Localized skin necrosis at heparin injection sites
Tip
HIT more commonly manifests with symptoms of thrombosis than with bleeding
Diagnostics
Differential diagnostics
- Nonimmune heparin-associated thrombocytopenia (formerly called type 1 HIT)
- A transient and clinically insignificant mild to moderate thrombocytopenia, usually occurring within 5 days of heparin initiation
- Caused by a direct effect of heparin on platelet activation
- Not associated with an increased risk of thrombosis