Epidemiology
- Women: 15–44 years
Etiology
- Genetic predisposition
- HLA-DR2 and HLA-DR3 are commonly present in individuals with SLE.
- Genetic deficiency of classical pathway complement proteins (C1q, C2, C4) in approx. 10% of affected individuals
- Hormonal factors: Hyperestrogenic states (e.g., due to oral contraceptive use, postmenopausal hormonal therapy, endometriosis) are associated with an increased risk of SLE.
- Environmental factors
- Cigarette smoking and silica exposure increase the risk of developing SLE.
- UV light and EBV infection may trigger disease flares
- Ultraviolet rays and sun exposure lead to increased cell apoptosis
- Drugs such as procainamide or hydralazine (see “Drug-induced lupus erythematosus”)
Pathophysiology
- Autoantibody development: deficiency of classical complement proteins (C1q, C4, C2) → failure of macrophages to phagocytose immune complexes and apoptotic cell material (i.e., plasma and nuclear antigens) → dysregulated, intolerant lymphocytes targeting normally hidden intracellular antigens → autoantibody production (e.g., ANA, anti-dsDNA)
- Normally, apoptotic cells are engulfed by macrophages during apoptosis, avoiding the release of intracellular content that induces inflammation or an immune response in the extracellular environment.
- Autoimmune reactions
- Type III hypersensitivity (most common in SLE) → antibody-antigen complex formation in microvasculature → complement activation and inflammation → damage to skin, kidneys, joints, small vessels
- Type II hypersensitivity → IgG and IgM antibodies directed against antigens on cells (e.g., red blood cells) → cytopenia
Clinical features
- SLE is a systemic disease characterized by phases of remission and relapse.
- SLE can affect any organ.
Common
- Constitutional: fatigue, fever, weight loss
- Joints (> 90% of cases)
- Arthritis and arthralgia
- Distal symmetrical polyarthritis: most commonly affects the joints of the fingers, carpal joints, and the knee
- Skin (85% of cases)
- Malar rash (butterfly rash): flat or raised fixed erythema over both malar eminences (nasolabial folds tend to be spared)
- Raynaud phenomenon
- Photosensitivity → maculopapular rash
- Ultraviolet rays and sun exposure lead to increased cell apoptosis

- Ultraviolet rays and sun exposure lead to increased cell apoptosis
- Discoid rash
- Oral ulcers (usually painless)
- Nonscarring alopecia (except with discoid rashes)
- Periungual telangiectasia
Tip
Both rheumatoid arthritis and SLE arthritis affect the MCP and PIP joints, but SLE does not usually lead to deformities.
Less common
- Hematological: petechiae, pallor, or recurrent infections due to cytopenias
- Warm AIHA, IgG causes extravascular hemolysis.
- Kidneys: nephritis with proteinuria (see “Lupus nephritis”)
- Mesangial and/or subendothelial deposition of immune complexes (e.g., anti-dsDNA antibodies, anti-Sm antibodies) → expansion and thickening of mesangium, capillary walls, and/or glomerular basement membrane
- Heart
- Pericarditis, myocarditis, endocarditis (Libman-Sacks endocarditis)
- Aortic valve lesions (e.g. Mitral valve prolapse)
- Coronary artery disease
Diagnostics
Laboratory studies
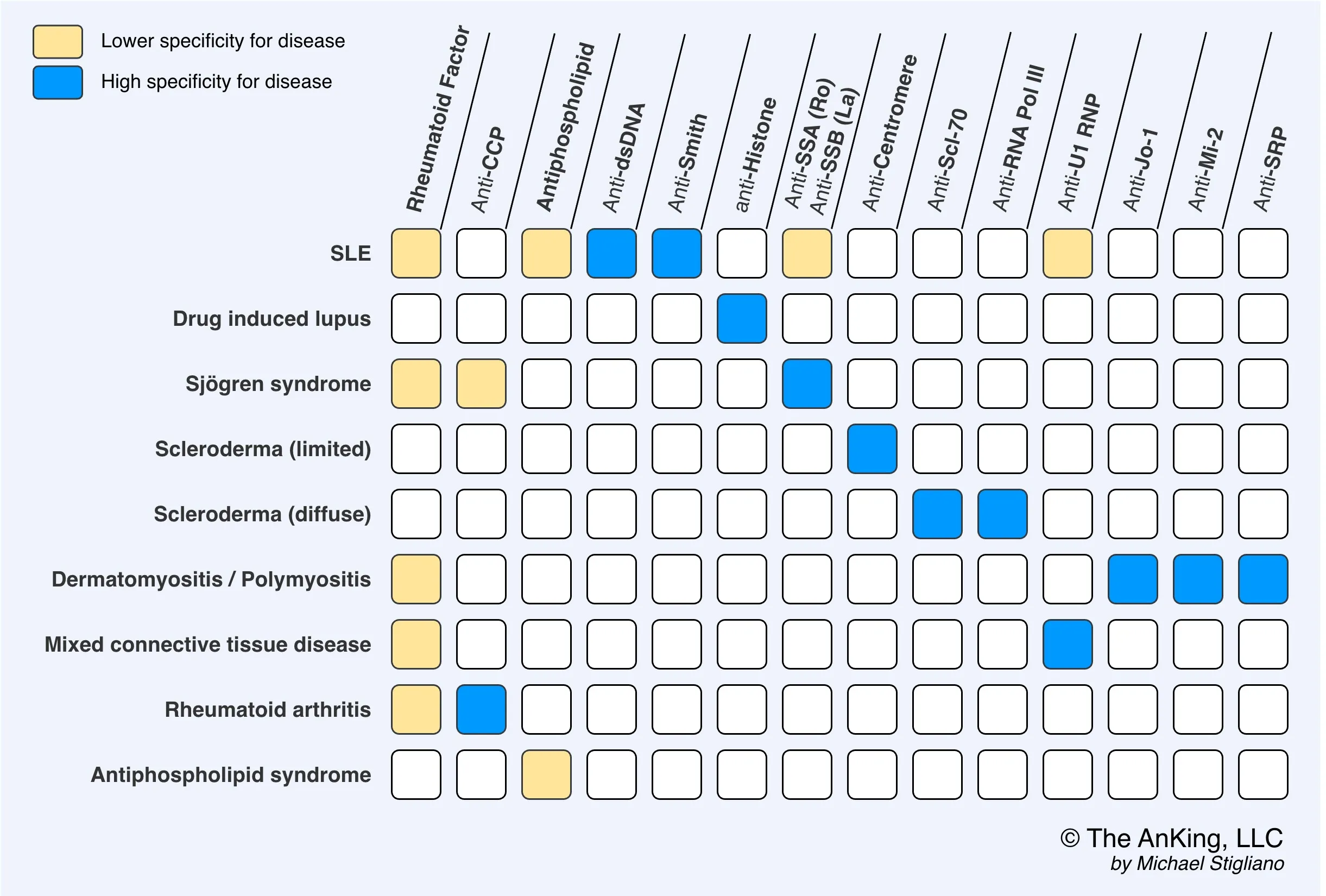
- Antinuclear antibodies (ANAs)
- Positive titers of ≥ 1:80 have ∼ 98% sensitivity for SLE
- Antigen-specific ANAs: Request only if ANAs are positive.
- Anti-dsDNA antibodies
- Autoantibodies against double-stranded DNA
- Positive in 60–70% of patients
- Highly specific for SLE
- Levels correlate with disease activity (especially lupus nephritis activity).
- Anti-Sm antibodies
- Autoantibodies against Smith antigens (nonhistone nuclear proteins)
- Smith can bond to snRNAs to form snRNPs, which can form a spliceosome.
- Positive in < 30% of patients, but highly specific for SLE
- Autoantibodies against Smith antigens (nonhistone nuclear proteins)
- Anti-dsDNA antibodies
- Antiphospholipid antibodies: Screen all patients for antiphospholipid syndrome.
- Laboratory markers of disease activity and/or organ damage in SLE
- Complement levels: ↓ C3 and/or ↓ C4 in patients with active disease, factor B levels remain normal
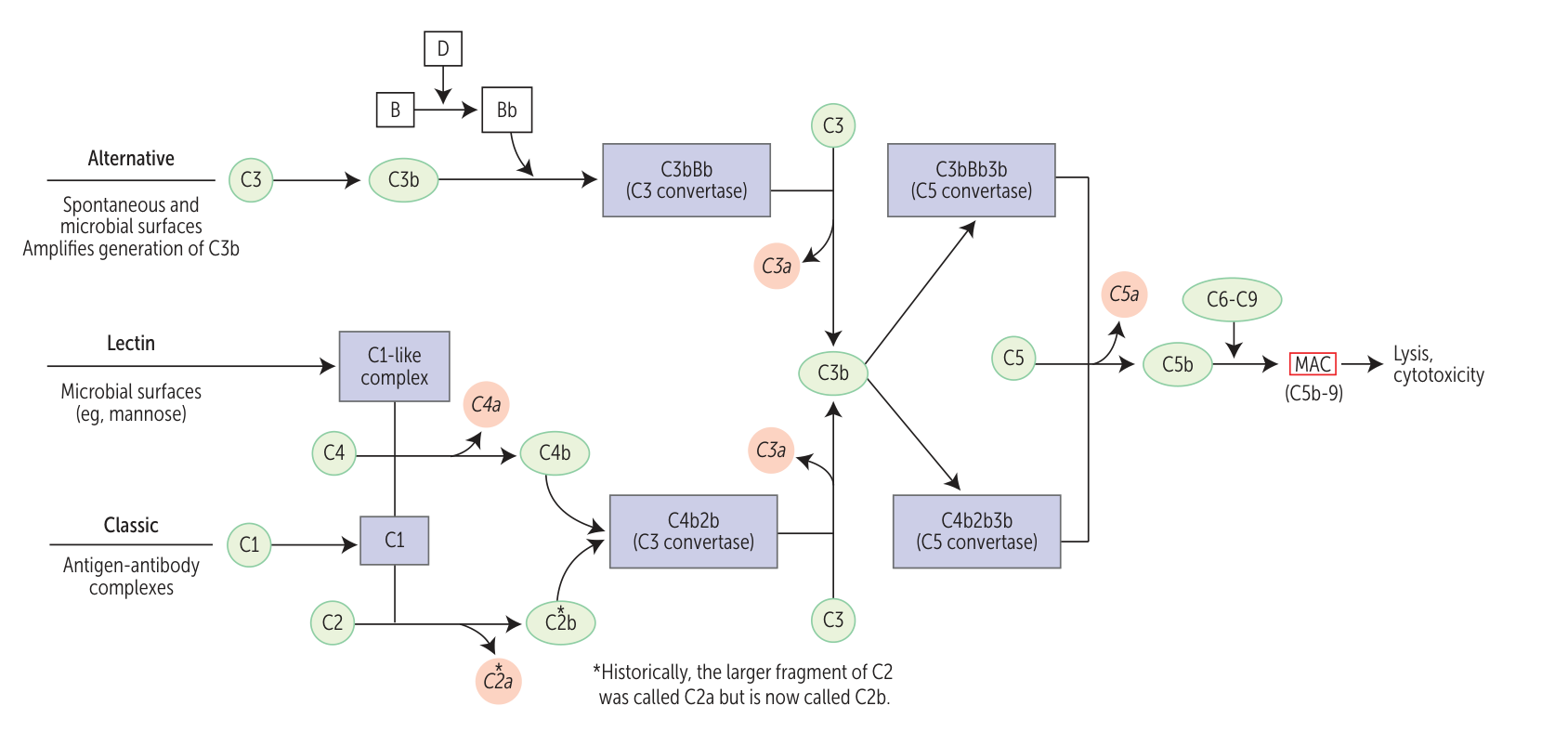
- Antigen-antibody complexes trigger classic pathway, which decreases C3 and C4. But factor B in alternative pathway is intact.
- Inflammatory markers
- ESR: may be elevated in patients with active disease
- CRP: often normal (may be elevated in patients with serositis, arthritis, or infections)
- CBC: may show leukopenia, thrombocytopenia, and/or autoimmune hemolytic anemia or anemia of chronic disease
- CMP: may show ↑ BUN and/or creatinine, and/or electrolyte abnormalities
- Urinalysis and urine microscopy: may show proteinuria, hematuria, and/or urinary casts
- Complement levels: ↓ C3 and/or ↓ C4 in patients with active disease, factor B levels remain normal
Tip
RPR and VDRL are usually used to test for syphilis but may also be positive in SLE. This happens in antiphospholipid syndrome as well.
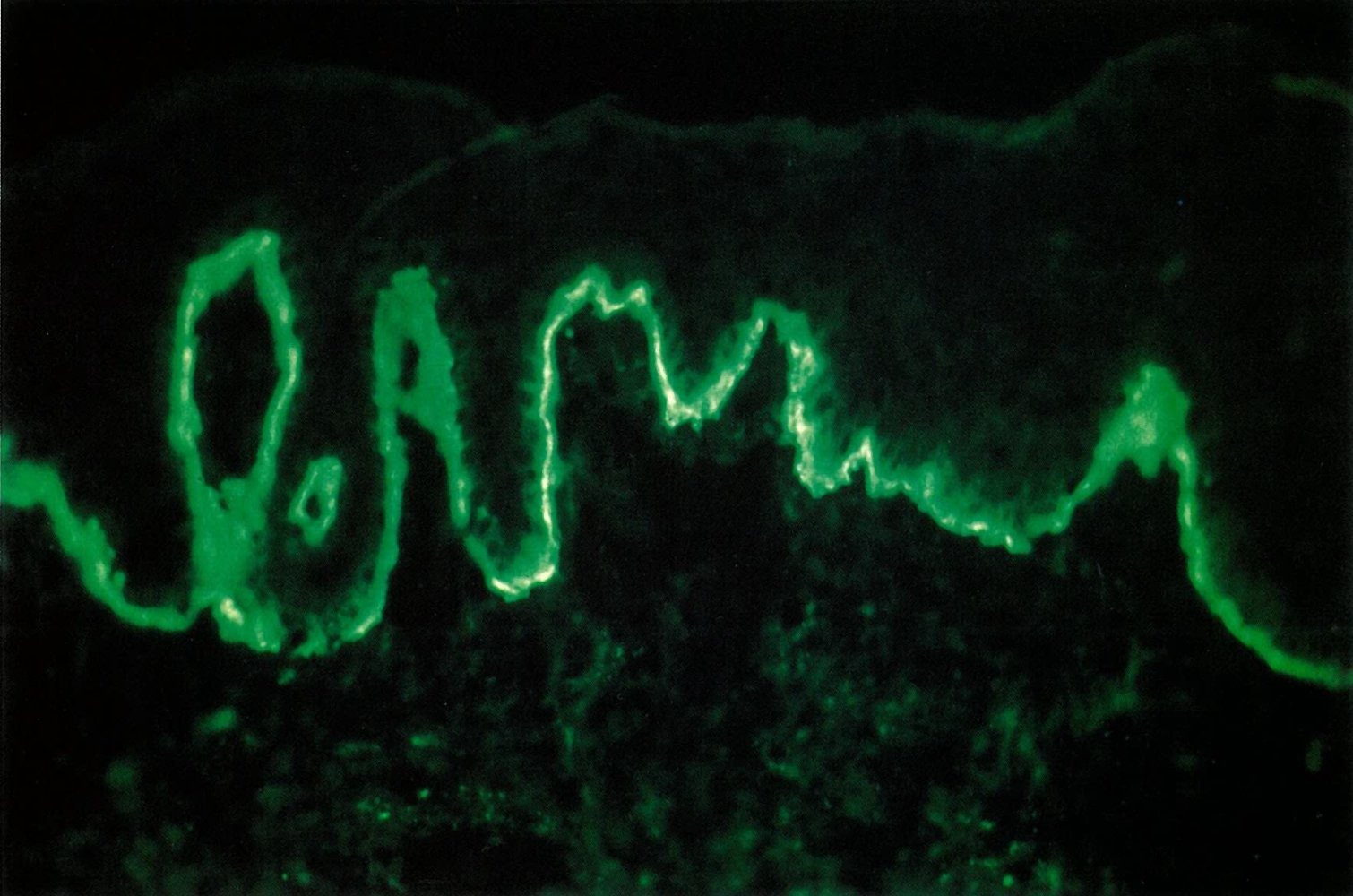
Skin biopsy
- Lupus band test (LBT): a direct immunofluorescence staining technique used to detect immunoglobulin and complement component deposits along the dermoepidermal junction in affected and unaffected skin in patients with SLE
Treatment
Complications
Cardiovascular disease
- ↑ Risk of thrombosis in all patients with SLE (especially if secondary antiphospholipid syndrome is present)
- ↑ Risk of myocardial infarction and stroke because of accelerated atherosclerosis