Epidemiology
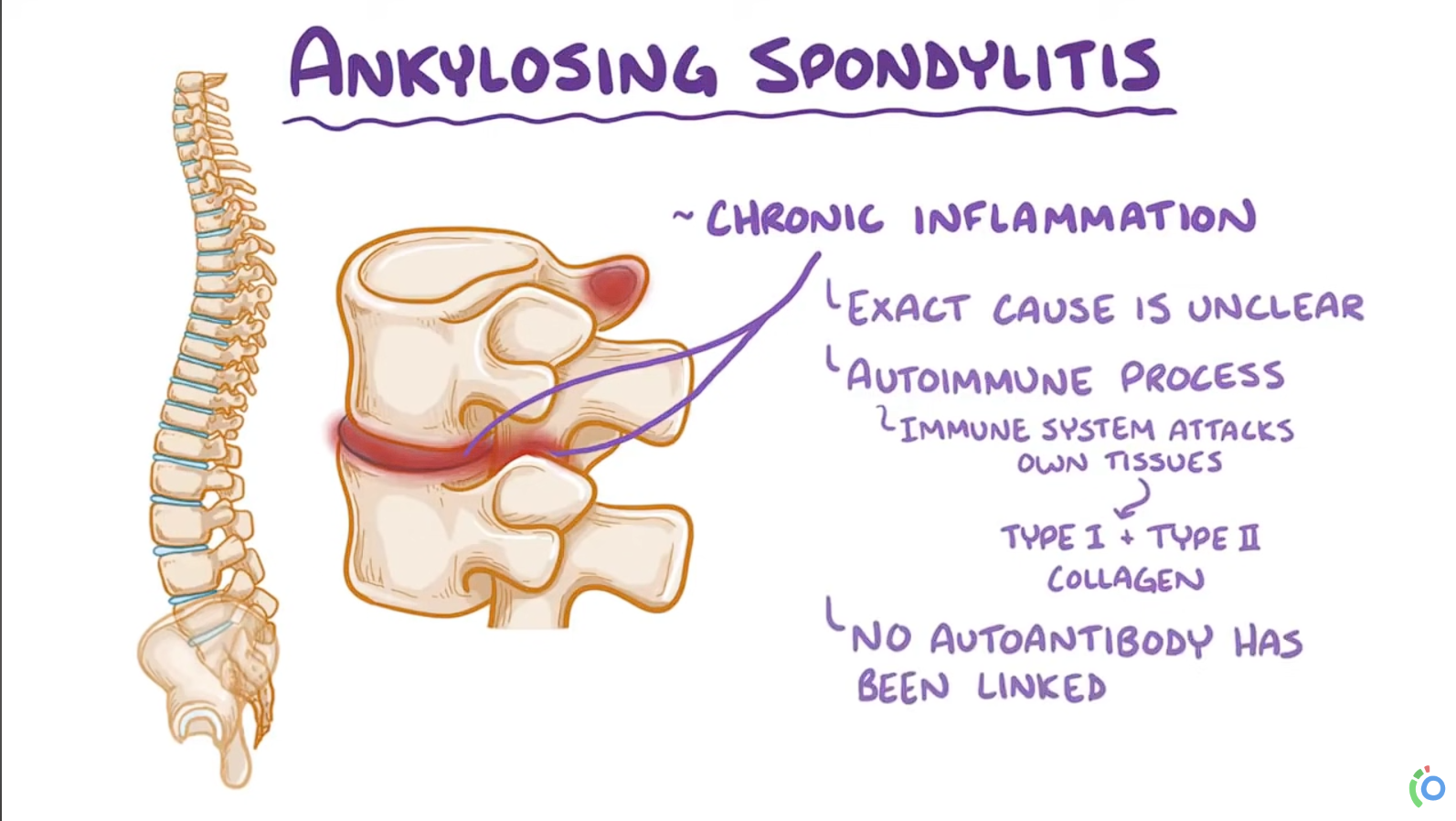
Etiology
- Genetic predisposition: 90–95% of patients are HLA-B27 positive.
Pathophysiology
- Initiation of innate immune response
- Release of cytokines (TGF-beta and TNF-α) and interleukins (IL-17 and IL-23)
- Infiltration of paravertebral and sacroiliac entheses with macrophages, CD4 T cells, and CD8 T cells
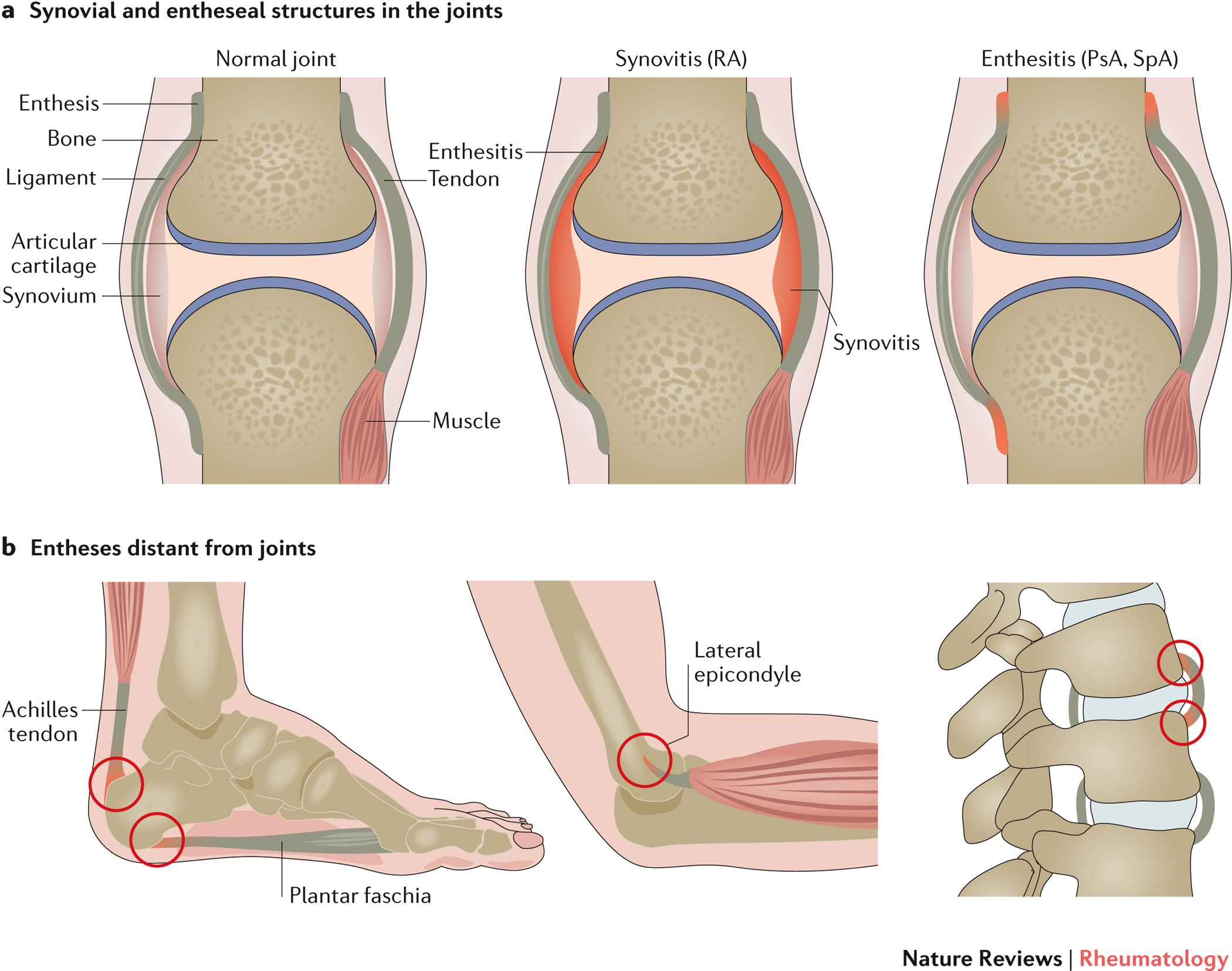
- Enthesitis: an inflammation of the enthesis (the point at which a tendon attaches to bone). Typically seen in patients with ankylosing spondylitis, psoriatic arthritis, enthesitis-associated juvenile idiopathic arthritis, or reactive arthritis. Commonly affected sites include the spine, Achilles tendon, plantar fascia, and supraspinatus tendon.
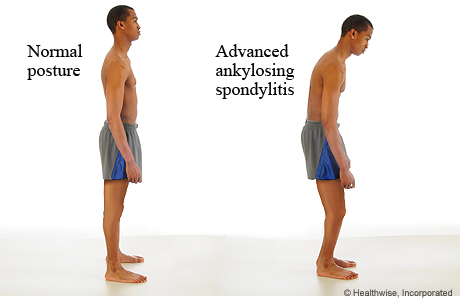
- Chronic enthesitis leads to:
- Erosion of the iliac part of the sacroiliac joints
- Vertical formation of syndesmophytes along the spinal ligament or around the annulus fibrosus of the intervertebral discs
- Fusion of syndesmophytes → ankylosis of intervertebral discs and vertebral bodies
Clinical features
- Inflammatory back pain (sacroiliitis)
- Insidious onset at age <40
- Morning stiffness > 30 minutes that improves with activity
- Pain is independent of positioning
- Relieved with exercise, worse with rest (overnight & in the morning)
- Relieved with activity & warm showers
- Nocturnal pain
- Reduced chest expansion & spinal mobility
- Stiff or stooped posture
- Tenderness at spine, sacroiliac joints & peripheral tendon insertions (eg, Achilles)
- Enthesitis (tenderness at tendon insertion sites)
- Dactylitis (swelling of fingers & toes)
- Uveitis
Diagnostics
AS is a seronegative spondyloarthropathy, and there are no serologic tests to confirm the diagnosis.
Laboratory findings
- Elevated ESR & CRP
- HLA-B27: Positive in 90–95% of patients with axial spondyloarthritis
- Autoantibodies (e.g., rheumatoid factor, antinuclear antibodies) are negative
X-ray
- Sacroiliitis: bone erosions, subchondral sclerosis, eventual bony fusion (ankylosis)
- Bridging syndesmophytes: ossification at vertebral body margins (bamboo spine)