Associated with Thymoma.
Pathophysiology
Thymus involvement
- Muscle-like (myoid) cells in the thymus express AChR → autoreactive targeting by T cells → production of acetylcholine receptor antibodies (AChR antibodies)
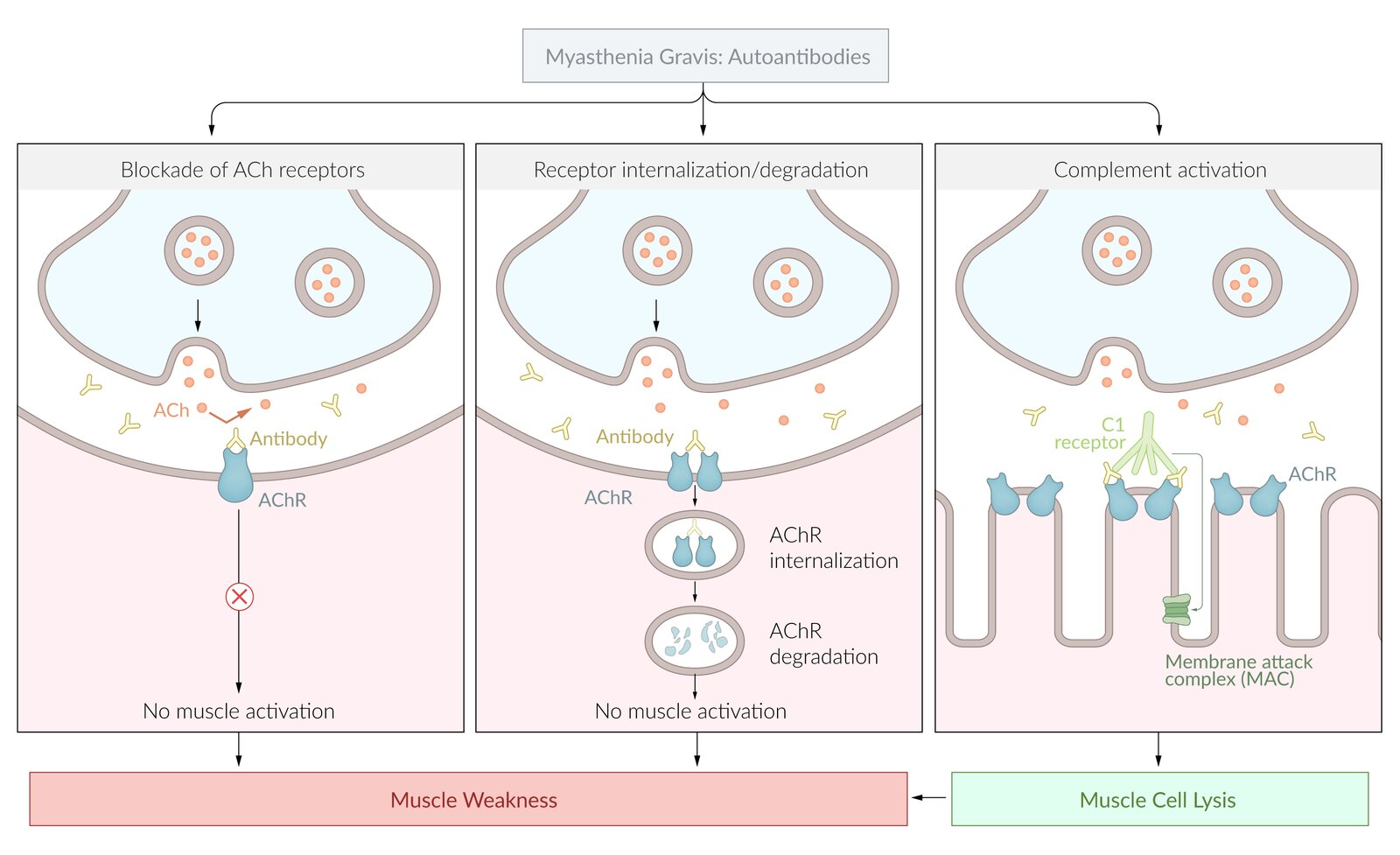
Acetylcholine receptor antibodies
- Responsible for inhibition of signal transduction at the neuromuscular junction (NMJ)
- Antibodies target postsynaptic AChRs of normal muscle cells → competitive inhibition of acetylcholine (ACh) → AChR decay through receptor internalization (↓ receptor density at the postsynaptic membrane) and activation of complement (→ muscle cell lysis) → impaired signal transduction at the NMJ → skeletal muscle weakness and fatigue
- Seropositive MG (80–90% of cases): positive assays for antibodies (in blood) against the acetylcholine receptor (AChR-Ab)
- Seronegative MG (10–20% of cases): negative for AChR antibodies, but may be positive for muscle-specific tyrosine kinase antibodies (MuSK antibodies)
Diagnostics
- Initial test: anti-AChR antibodies (highly specific for MG)
Warning
Because MG and LEMS are neuromuscular junction disorders, muscle biopsy of these conditions will be normal. Unlike in myopathies (e.g. Polymyositis, Dermatomyositis, Mitochondrial myopathies)
Differential diagnostics
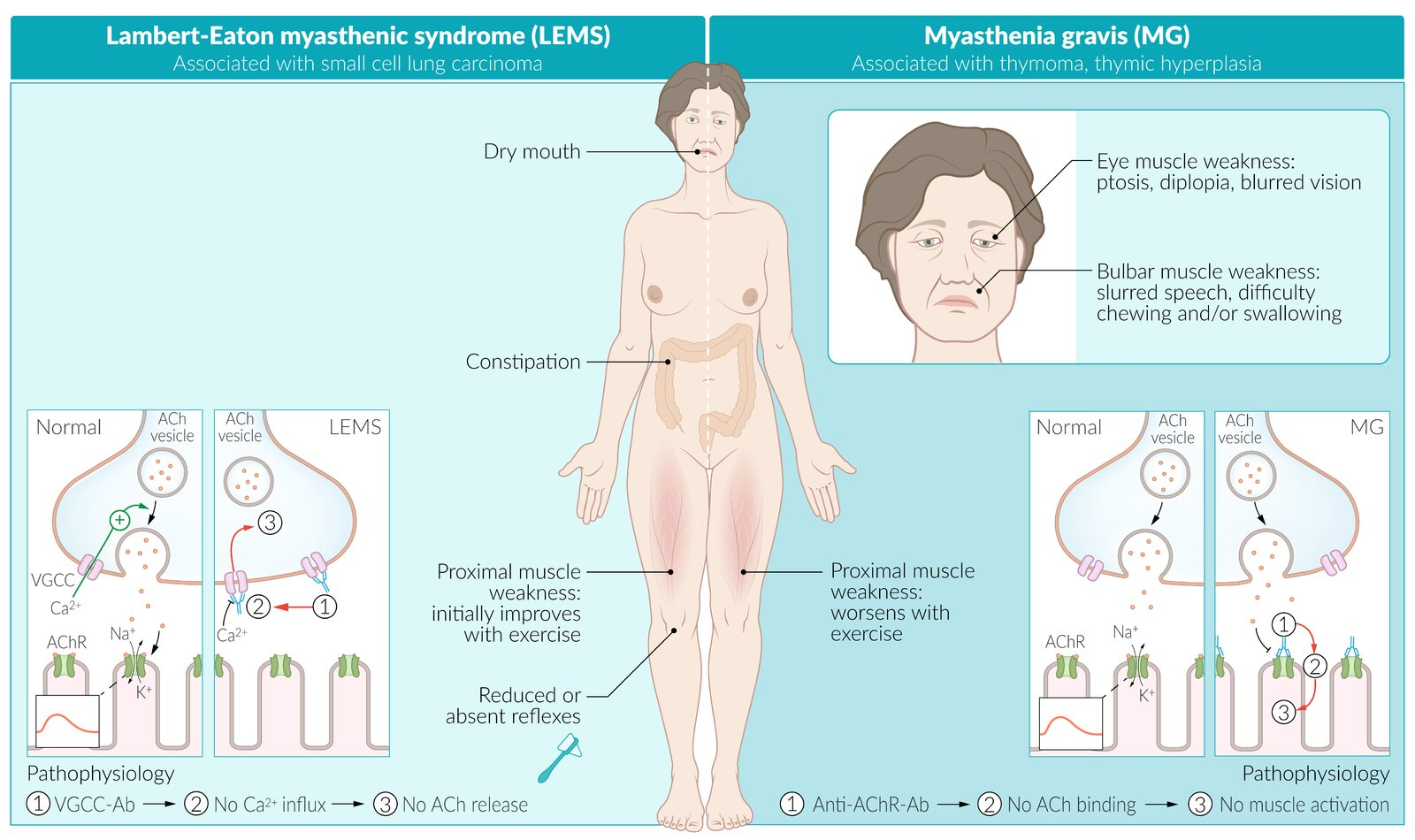
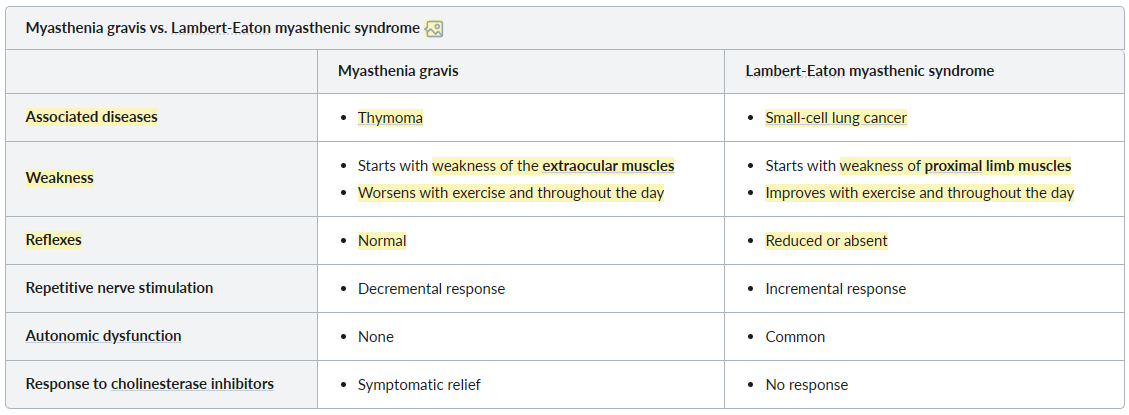
Lambert-Eaton myasthenic syndrome (LEMS)
- Etiology
- Paraneoplastic: associated with small-cell lung carcinoma (in ⅔ of patients with LEMS)
- Pathophysiology: autoantibodies directed against presynaptic voltage-gated calcium channels (anti-VGCC antibodies) → ↓ Ca2+ influx → ↓ presynaptic vesicle fusion → impaired acetylcholine release in the NMJ
Tip
- Extraocular muscles: move frequently, so they are first affected.
- MG: Repeated nerve stimulation → decreasing ACh release (as the storage is limited) → worsen symptoms
- LEMS: More depolarization → more ACh release → improved symptoms