Epidemiology
Etiology
- Primary hypothyroidism: insufficient thyroid hormone production
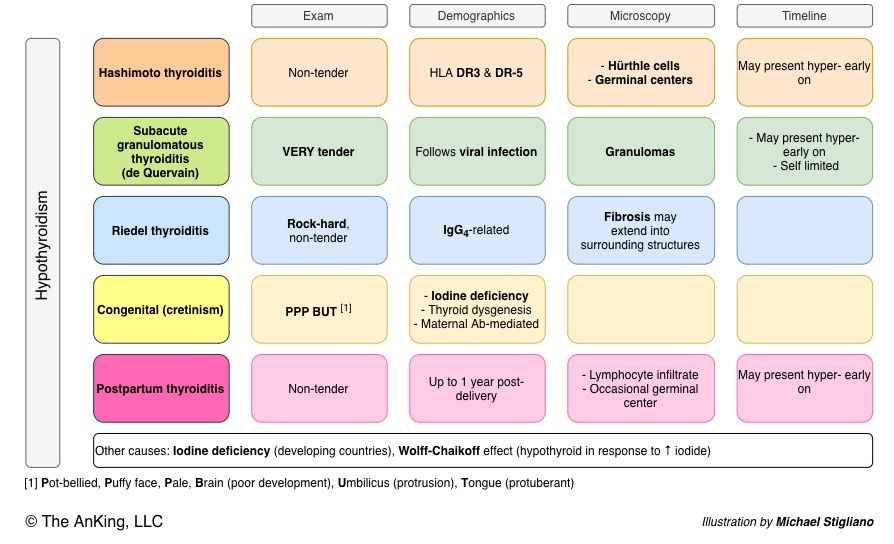
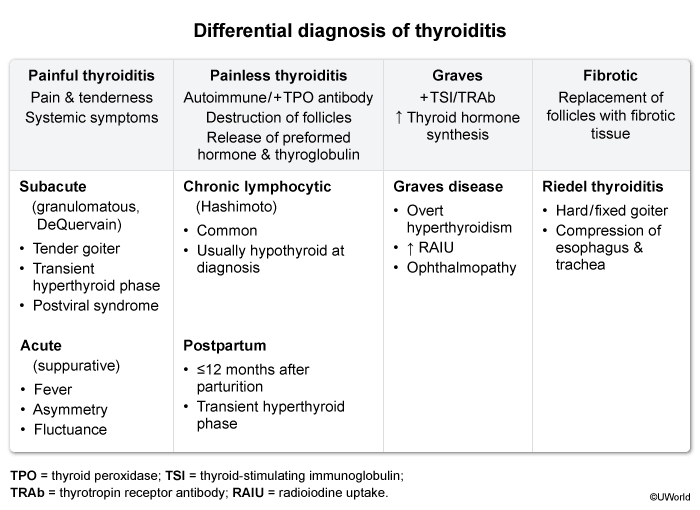
- Hashimoto thyroiditis
- The most common cause of hypothyroidism in iodine-sufficient regions
- Associated with HLA-DR3 and other autoimmune diseases (e.g., vitiligo, pernicious anemia, type 1 diabetes mellitus, and systemic lupus erythematosus)
- Postpartum thyroiditis (subacute lymphocytic thyroiditis)
- De Quervain thyroiditis (subacute granulomatous thyroiditis): often subsequent to a flu-like illness
- Iatrogenic: e.g., post thyroidectomy, radioiodine therapy, antithyroid medication (e.g., amiodarone, lithium)
- Nutritional (insufficient intake of iodine): the most common cause of hypothyroidism worldwide, particularly in iodine-deficient regions
- Riedel thyroiditis: occurs in IgG4-related systemic disease
- Wolff-Chaikoff effect
- Thyroid dysplasia: a disorder of embryologic development characterized by abnormal development and/or location of thyroid tissue (e.g., lingual thyroid)
- Hashimoto thyroiditis
- Secondary hypothyroidism: pituitary disorders (e.g., pituitary adenoma) → compression of normal cells (mass effect) → TSH deficiency
- Tertiary hypothyroidism: hypothalamic disorders → TRH deficiency
Pathophysiology
Clinical features
- Symptoms related to decreased metabolic rate
- Hair loss (Queen Anne sign), brittle nails, and cold, dry skin
- Weight gain (despite poor appetite)
- Symptoms related to generalized myxedema
- Hoarse voice, difficulty articulating words
- Symptoms of hyperprolactinemia
- Abnormal menstrual cycle (esp. secondary amenorrhea or menorrhagia)
- Galactorrhea
- Decreased libido, erectile dysfunction, delayed ejaculation, and infertility in men
Diagnostics
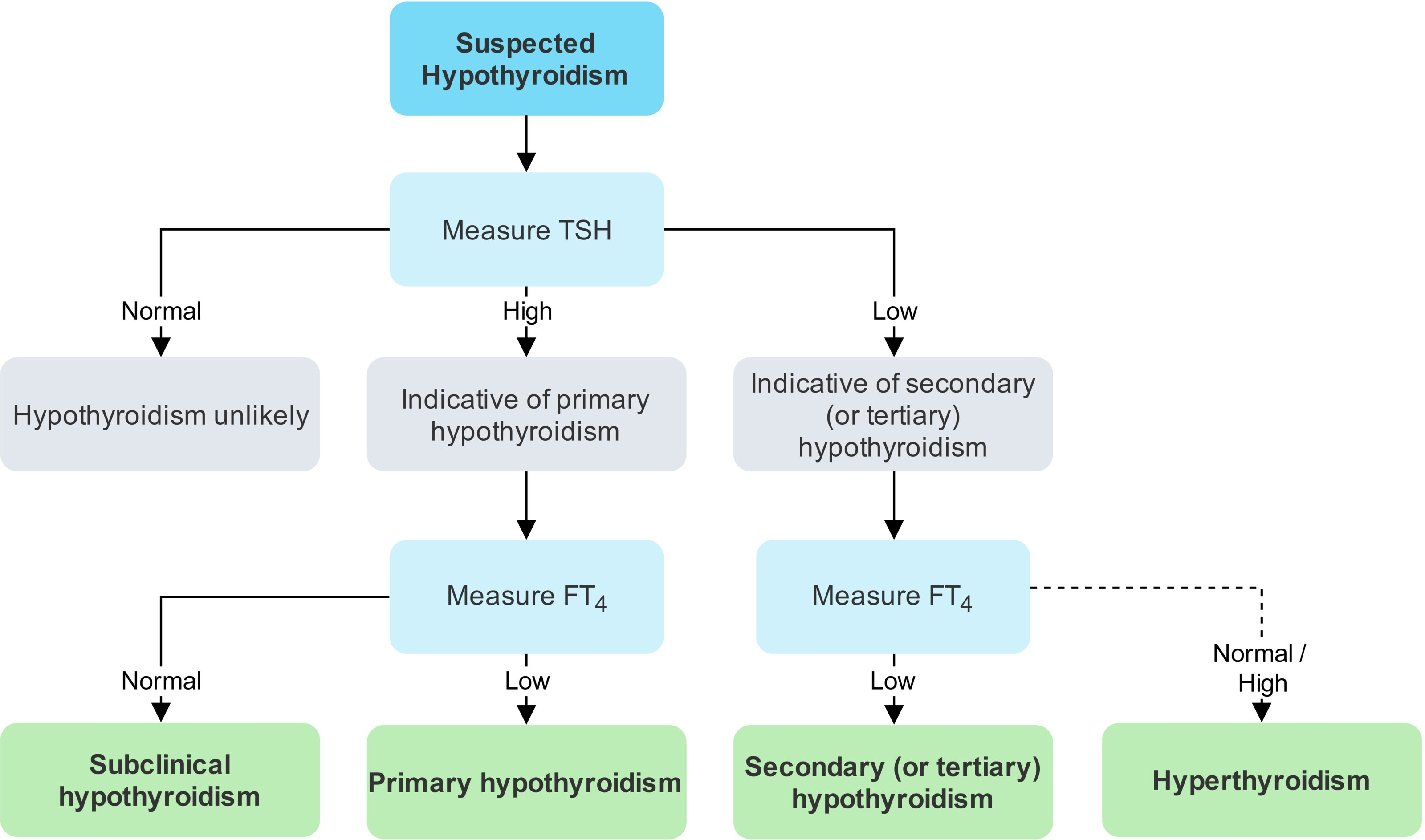
- Screening: TSH is the most sensitive test. t
- Thyroid hormone suppresses TSH and TRH via negative feedback, and small changes in thyroid hormone levels lead to large changes in TSH levels. As thyroid hormone production slows, TSH secretion increases rapidly to restore thyroid activity, often before T4 levels fall below standard laboratory reference ranges.
- Primary Hypothyroidism: ↑ TSH, ↓ Free T4. The pituitary gland tries to stimulate a failing thyroid.
- Subclinical Hypothyroidism: ↑ TSH, Normal Free T4. Patients may be asymptomatic or have mild symptoms. Often an early stage of Hashimoto’s.
- Central Hypothyroidism: ↓ or inappropriately normal TSH, ↓ Free T4.
- Antibodies: Anti-TPO antibodies to confirm Hashimoto’s thyroiditis.
Treatment
Hypothyroidism is treated with lifelong hormone substitution.
- Levothyroxine: synthetic form of T4
- First-line choice for the treatment of hypothyroidism
- Peripherally converted to T3 (biologically active metabolite) and rT3 (biologically inactive metabolite)
- In patients with severe Euthyroid Sick Syndrome, aka non-thyroidal illnesses (like sepsis or major trauma), rT3 levels often rise while active T3 levels fall, even if TSH is normal or low.
- Administration: Take on an empty stomach (e.g., 30-60 min before breakfast) as iron, calcium, and antacids can decrease absorption.
- Liothyronine: synthetic form of T3
- Part of the treatment for myxedema coma
- Not recommended as monotherapy or in combination with levothyroxine for the long-term treatment of hypothyroidism
- Liothyronine has a short half-life and requires three to four daily doses, making it less suitable than levothyroxine for the ongoing treatment of hypothyroidism.
Mnemonic
T4 (levothyroxine; levo = 4 letters) or T3 (liothyronine; lio = 3 letters)
Congenital hypothyroidism
Pathophysiology
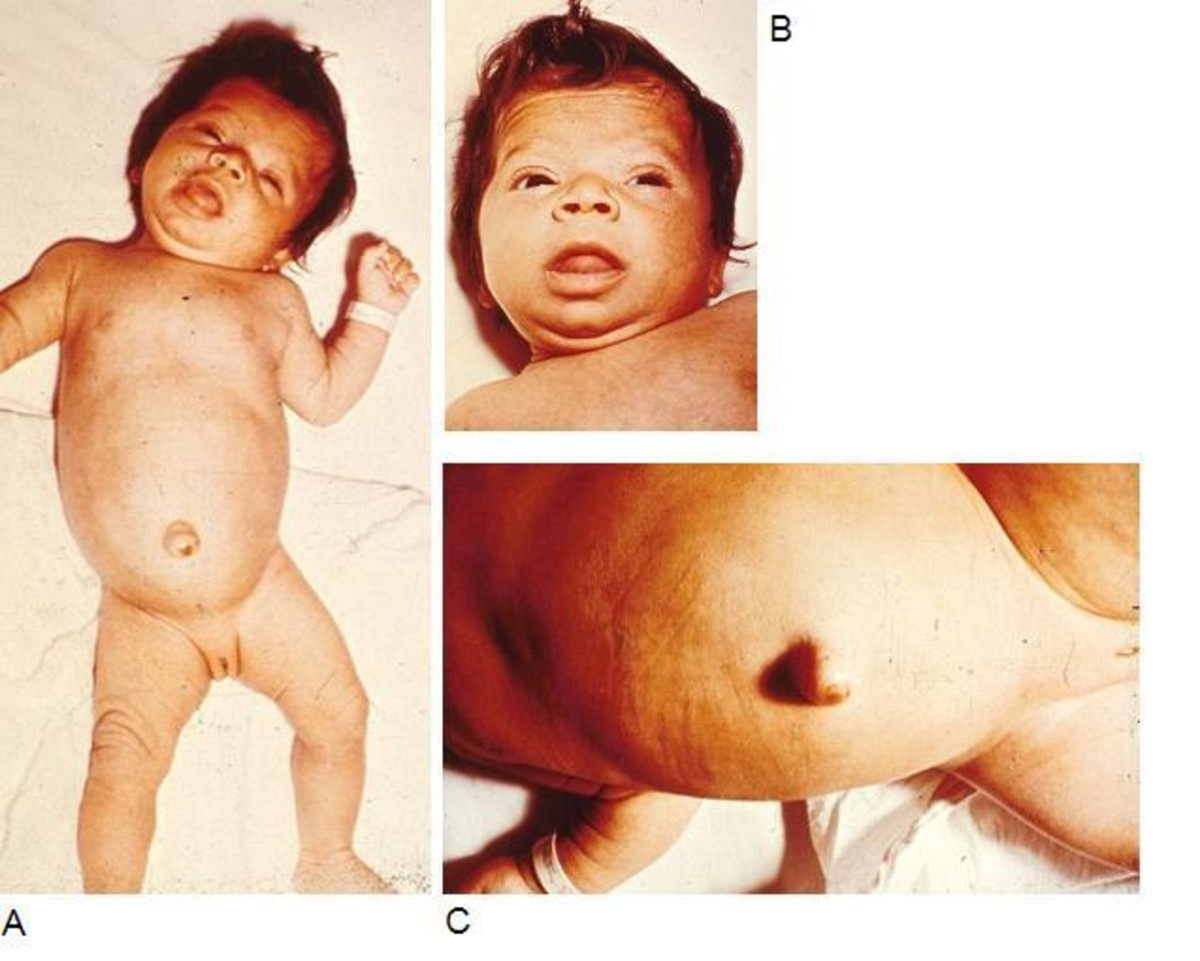
- Puffy Face, Macroglossia, Hoarse Cry t
- Accumulation of Glycosaminoglycans (GAGs) (e.g., hyaluronic acid) within interstitial spaces osmotic water retention (Myxedema).
- Prolonged Jaundice
- ↓ T4 decreased activity of hepatic UDP-glucuronyl transferase impaired bilirubin conjugation.
- Intellectual Disability
- Thyroid hormone is essential for CNS myelination and synaptogenesis; deficiency causes irreversible neuronal damage.
- Umbilical Hernia & Pot-Belly t
- Due to generalized hypotonia (abdominal muscle weakness).
- Large Fontanelles & Short Stature
- ↓ T4 Delayed skeletal maturation (impairs ossification centers).
- Constipation, Lethargy, Cold Intolerance
- ↓ T4 ↓ Basal Metabolic Rate (BMR) and decreased sympathetic sensitivity.
Clinical features
- Most infants are asymptomatic at birth due to maternal T4 crossing the placenta.
- Symptoms develop over weeks to months if untreated.
- Classic “Cretinism” features:
- 6 P’s: Pot-bellied, Pale, Puffy-faced, Protruding umbilicus (umbilical hernia), Protuberant tongue (macroglossia), Poor brain development.
- Other findings: Lethargy, poor feeding, prolonged jaundice, constipation, hoarse cry, hypotonia, and large fontanelles.
Warning
Most children with congenital hypothyroidism do not have symptoms at the time of birth because the placenta supplies the fetus with maternal thyroid hormone. For this reason, neonatal screening is vital even if children are asymptomatic. Irreversible intellectual disabilities can be avoided through early initiation of adequate therapy!
Diagnostics
- Neonatal screening to measure TSH levels 24–48 hours after birth is required by law.
- Increased TSH levels indicate congenital hypothyroidism.
| Feature | Congenital Hypothyroidism (CH) | Down Syndrome (DS) |
|---|---|---|
| Onset | Develops weeks after birth (initially normal) | Features present at birth |
| Face | Coarse, puffy features, large fontanelles | Flat profile, upslanting palpebral fissures |
| Abdomen | Umbilical hernia, pot-belly, constipation | Associated w/ duodenal atresia |
| Hands/Feet | Normal | Single palmar crease, sandal gap |
| Tone | Hypotonic & lethargic | Profoundly hypotonic |
| Skin | Prolonged jaundice, dry/mottled skin | Normal skin texture |
| Eyes | Normal structure | Brushfield spots on iris |