Etiology
Tip
Bronchiectasis requires the combination of two important processes taking place in the bronchi:
- either local infection
- or inflammation along with either inadequate clearance of secretions, airway obstruction, or impaired host defenses.
These processes result in the permanent dilation of airways.
- Pulmonary infections (i.e., bacterial, viral, fungal), especially severe or chronic infections
- Disorders of secretion clearance or mucous plugging
- Cystic fibrosis (CF) (Most common congenital cause of bronchiectasis)
- Primary ciliary dyskinesia (PCD)
- Allergic bronchopulmonary aspergillosis (ABPA)
- Kartagener syndrome
- Smoking: associated with poor ciliary motility
- Bronchial narrowing or other forms of obstruction
- COPD
- Aspiration
- Tumors
- Immunodeficiency (e.g., common variable immunodeficiency, hypogammaglobulinemia, HIV)
Pathophysiology
Clinical features
- Chronic productive cough (lasting months to years) with copious mucopurulent sputum
- The sputum may be green or yellow in color.
- Auscultation
- Crackles and rhonchi
- Wheezing
- Dyspnea
- Hemoptysis: usually mild or self-limiting, but severe hemorrhage that requires embolization may occur
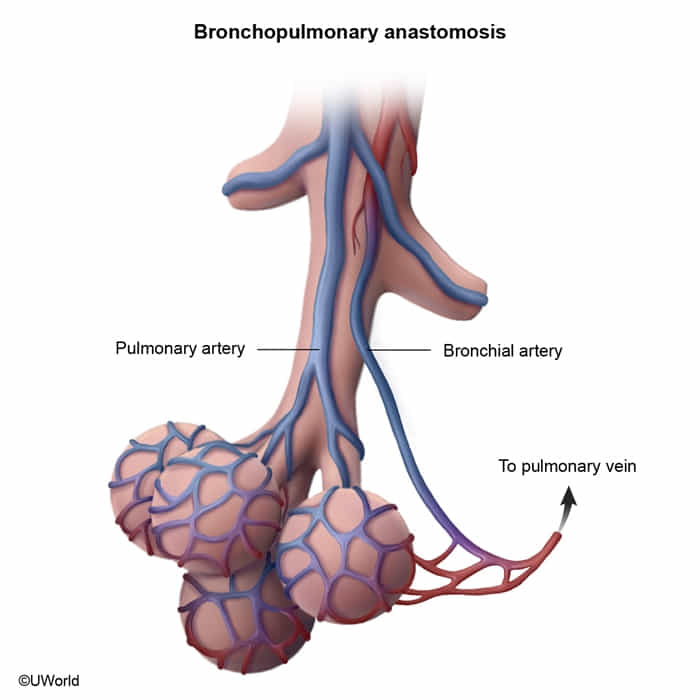
- Results from the rupture of dilated bronchial wall vessels (not pulmonary vessels)
- Chronic and recurrent airway inflammation and infection stimulates neovascularization and bronchial artery hypertrophy. The dilated, fragile, and tortuous vessels are in close proximity to the bronchioles and prone to rupture with increased airway pressure, such as during coughing (eg, acute pulmonary exacerbation).
- Although bleeding from the low-pressure pulmonary circulation is more common, hemorrhage from the high-pressure, systemic bronchial circulation is usually responsible for massive, life-threatening hemoptysis.
- Exacerbations of bronchiectasis
- Recurrent bouts of pneumonia and acute bacterial infection of sections of dilated bronchi
- Frequently due to Pseudomonas aeruginosa
- Features
- Increased production of mucous above baseline
- Low-grade fever
Note
Bronchiectasis should be suspected in patients with a chronic cough that produces large amounts of sputum.
Diagnostics
Tip
In patients with suspected bronchiectasis, diagnosis is confirmed using imaging studies, preferably a HRCT scan. Additional diagnostic studies are useful to identify the underlying cause and possibly provide specific treatment.
Imaging
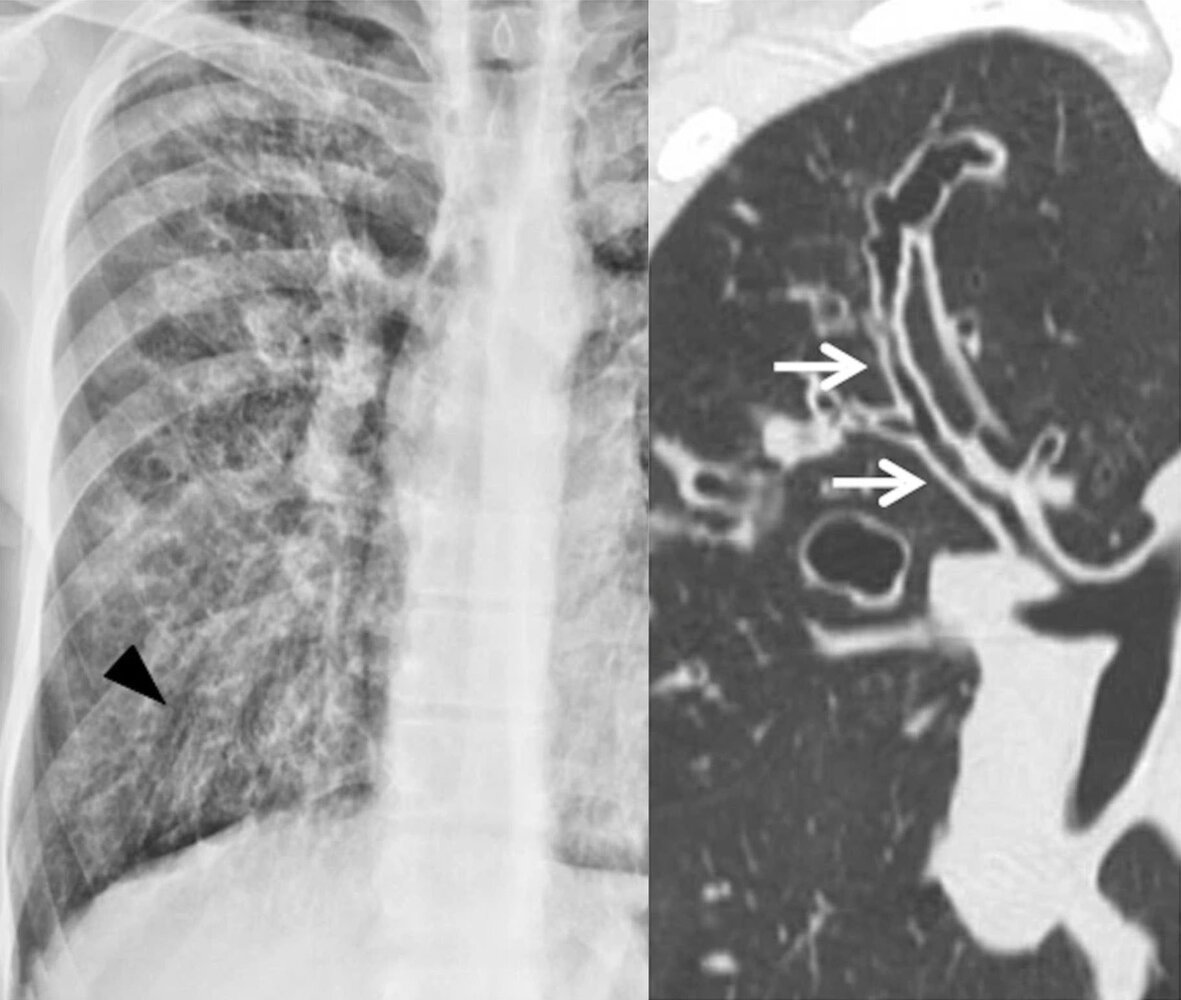
High-resolution computed tomography (HRCT) chest: confirmatory test
- Bronchial dilation
- Cylindrical or tubular (most common) : parallel tram track sign and signet ring sign
- Varicose
- Saccular or cystic (most severe form)
- Bronchial dilation can be identified with a bronchial/arterial ratio > 1 (normally < 1)

- Cylindrical or tubular (most common) : parallel tram track sign and signet ring sign
- Thickened bronchial walls, mucus plugging, honeycombing (suggests late-stage bronchiectasis)
Treatment
- Airway Clearance: Chest physiotherapy, postural drainage, positive expiratory pressure (PEP) devices.
- Antibiotics for Exacerbations: Guided by sputum cultures; often requires prolonged courses (10-14 days). Common empiric choices include amoxicillin-clavulanate or a fluoroquinolone.
- Chronic Suppressive Antibiotics: For patients with ≥3 exacerbations/year (e.g., macrolides like azithromycin).
- Bronchodilators: Inhaled beta-agonists for patients with airway hyperreactivity.
- Surgery (Lobectomy): For localized, severe bronchiectasis or massive hemoptysis.