Epidemiology
Etiology
- HCM is a genetic condition characterized by otherwise unexplained left ventricular hypertrophy.
- Most common hereditary heart disease
- Autosomal dominant inheritance with varying penetrance
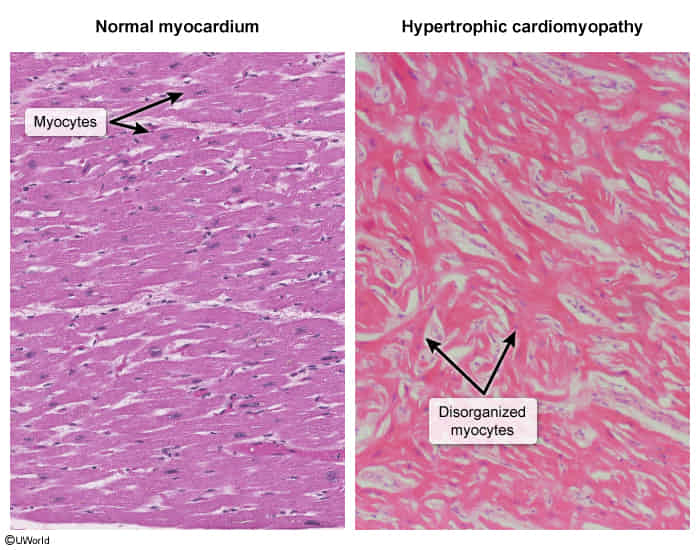
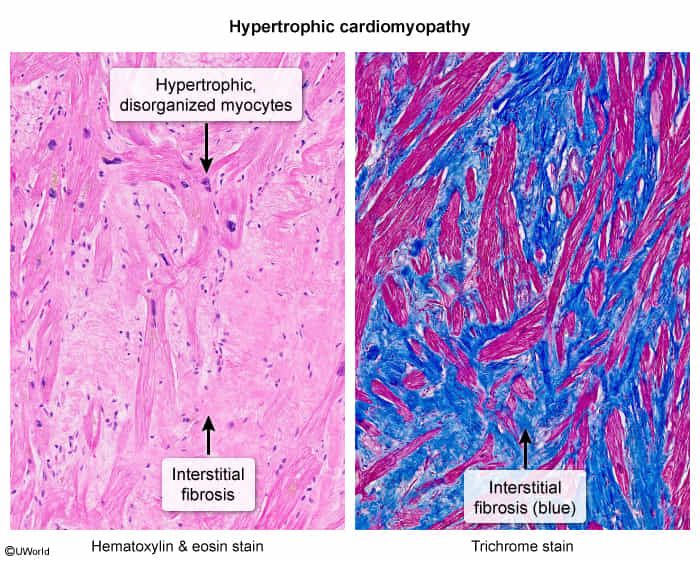
- Most commonly caused by mutations of the sarcomeric protein genes (e.g., myosin heavy chain, myosin binding protein C) → disorganization of myocyte architecture characterized by myofibrillar disarray and fibrosis
- Other conditions that are associated with left-ventricular hypertrophy include the following:
- Chronic hypertension (most common cause of left ventricular hypertrophy)
- Aortic stenosis
- Friedreich ataxia, Fabry disease, Noonan syndrome
- Amyloidosis
Pathophysiology
Tip
Hypertrophic cardiomyopathy shows localized, asymmetrical, rather than uniform, thickening of the LV walls, predominantly affecting the interventricular septum. This is different from hypertensive heart disease, which shows uniformly thickened left ventricular (LV) walls
HOCM
- Mechanisms of obstruction
- Systolic anterior motion (SAM) of the mitral valve, results in mitral-septal contact during mid-to-late systole ; caused by either or both:
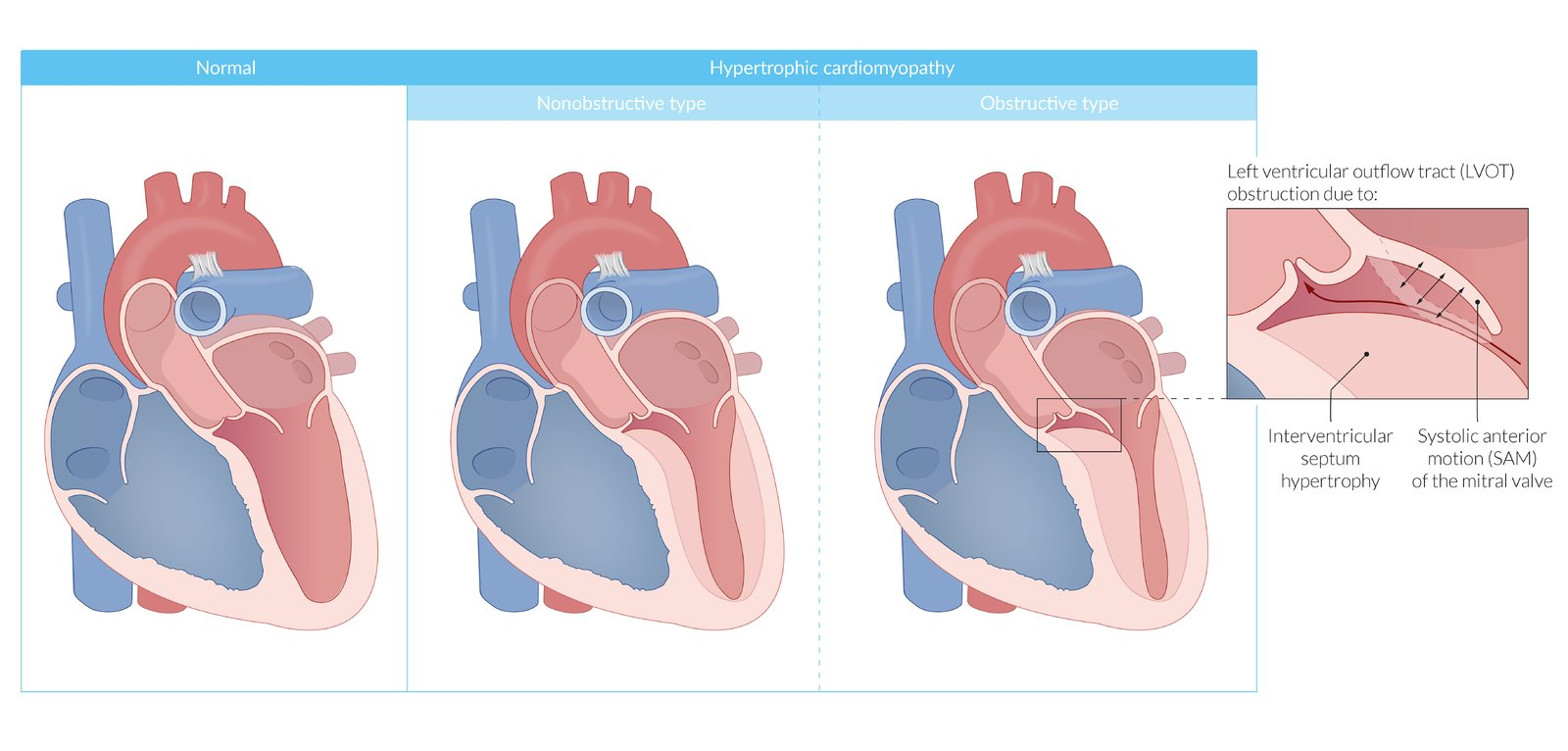
- Venturi effect: accelerated blood flow through ventricular outflow tract creates negative pressure that pulls the mitral valve towards the septum → increased outflow tract obstruction
- Ejection against an elongated and distorted mitral valve causes leaflets to get pulled into the outflow tract → potential secondary mitral regurgitation
- Muscular obstruction
- Encroachment of the LVOT by the hypertrophic septum
- Systolic anterior motion (SAM) of the mitral valve, results in mitral-septal contact during mid-to-late systole ; caused by either or both:
- LVOT obstruction is dynamic
- The following factors can increase the degree of obstruction: ↑ LV contractility, ↓ preload, and ↓ afterload
- Clinically exacerbating factors
- These factors lead to increased heart contraction force and cardiac output and, thus, enhance the ejection flow. This increases the Venturi effect force described above.
- Physical exercise/stress
- Dehydration
- Pharmacologic provocation (e.g., diuretics, ACEIs/ARBs, digoxin, hydralazine)
- Valsalva maneuver (strain phase)
- Leads to decreased preload
- Compare with Aortic stenosis, which alleviates upon Valsalva maneuver
Clinical features
- Symptoms: worsen with exercise, dehydration, and use of certain drugs (e.g., diuretics, hydralazine, ACEIs/ARBs, digoxin)
- Frequently asymptomatic (especially the nonobstructive type)
- Exertional dyspnea
- Angina pectoris
- Dizziness, lightheadedness, syncope
- Palpitations, cardiac arrhythmias
- Sudden cardiac death (particularly during or after intense physical activity)
- Physical examination
- Systolic ejection murmur (crescendo-decrescendo) at left sternal border
- Note the location is different from aortic stenosis, which is at right upper sternal border (the aortic area). This is because obstruction in the left ventricular outflow tract is below the aortic valve.
- Increases with Valsalva maneuver, standing, inotropic drugs (e.g., digitalis)
- Decreases with:
- Hand grip, squatting, or passive leg elevation
- Drugs that decrease cardiac contractility (e.g., beta blockers)
- Possible holosystolic murmur from mitral regurgitation
- Sustained apex beat
- S4 gallop
- Paradoxical split of S2
- Pulsus bisferiens: LV outflow obstruction causes a sudden quick rise of the pulse followed by a slower longer rise (biphasic pulse).
- Systolic ejection murmur (crescendo-decrescendo) at left sternal border
Tip
HOCM is an important cause of sudden cardiac death in young patients!