Etiology
- Most common: Deep vein thrombosis
- Causes of nonthrombotic embolism
- Fat embolism
- Air embolism
- Amniotic fluid embolism
- Bacterial embolism
- Patients with intravenous drug use are at increased risk of developing tricuspid valve endocarditis, giving rise to septic pulmonary emboli
- Others: pulmonary tumor embolism, pulmonary cement embolism
Tip
Up to 30% of cases may present with no apparent risk factors (eg, hypercoagulability).
Pathophysiology
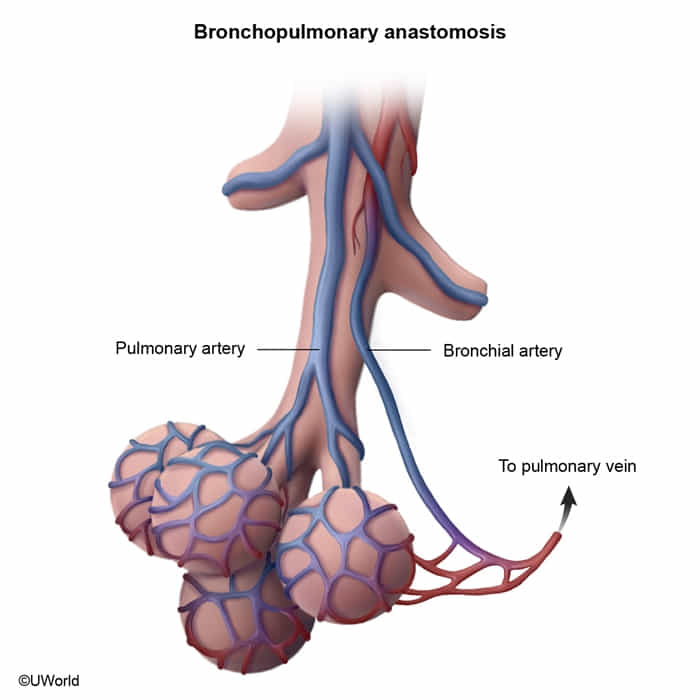
- The lung is supplied by dual circulation from both the pulmonary arteries and bronchial arteries. This collateral circulation can help protect against lung infarction as a complication of pulmonary embolism (PE).
- Distal PEs in small arteries (≤3 mm) are more likely to cause infarction as they may occlude areas distal to the pulmonary-bronchial anastomoses.
- When a pulmonary infarction does occur, it is typically hemorrhagic (red) rather than ischemic (white) due to the relatively low density of lung tissue and the dual blood supply.
Clinical features
- Common features of PE
- Acute onset of symptoms
- Dyspnea (> 75% of cases)
- Tachycardia and tachypnea (up to 50% of cases)
- Sudden pleuritic chest pain (∼ 20% of cases)
- Cough and hemoptysis
- Associated features of DVT: e.g., unilaterally painful leg swelling
- Features of massive PE (e.g., due to a saddle thrombus)
- Presyncope or syncope
- Jugular venous distension and Kussmaul sign
- RV pressure overload
- Hypotension and obstructive shock
- Circulatory collapse
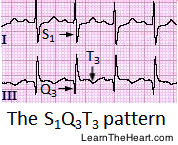
ECG
ECG changes may be due to right ventricular strain and pressure overload. Most common findings
- T-wave inversions or flattening
- Sinus tachycardia
- Normal ECG
- S1Q3T3 pattern (neither sensitive nor specific)
 Predictors of adverse outcomes: See “High-risk ECG findings in PE.”
Other ECG findings in PE: sinus bradycardia (< 60/min); uncommon)
Predictors of adverse outcomes: See “High-risk ECG findings in PE.”
Other ECG findings in PE: sinus bradycardia (< 60/min); uncommon)
Treatment
Reperfusion therapy
- Indications
- Massive PE (hemodynamic instability and/or right heart failure) with a low bleeding risk
- Recombinant tissue plasminogen activator (tPA), e.g., alteplase (preferred)
- Endothelial-derived TPA is limited primarily to the bronchial circulation, and spontaneous recanalization of the pulmonary artery is a slow process.