Epidemiology
Etiology
Exogenous risk factors
- Diet rich in nitrates and/or salts (e.g., dried foods, foods preserved by curing or smoking) and low in fresh vegetables containing antioxidants t
- Bacteria are believed to convert ingested nitrates into carcinogenic nitrites.
- H. pylori infection
- Nicotine use
- Epstein-Barr virus
Endogenous risk factors
- Gastric conditions
- Chronic atrophic gastritis and associated pernicious anemia
- Achlorhydria (e.g., due to Ménétrier disease)
- Gastric ulcers
Pathophysiology
Two major histologic types
- Intestinal Type
- Resembles colonic adenocarcinoma; forms glandular structures.
- Located typically on the lesser curvature of the antrum/pylorus.
- Strong association with H. pylori, smoking, and nitrosamines.
- Diffuse Type
- Not associated with H. pylori.
- Signet Ring Cells: Mucin-filled cells with nucleus pushed to the periphery.
- Linitis Plastica: “Leather bottle” stomach due to diffuse infiltration and thickening of the stomach wall (loss of distensibility).
- Younger patients; worse prognosis.
Clinical features
Diagnostics
Pathology
Gastric adenocarcinoma
- Accounts for ∼ 95% of cases
- Most commonly located on the lesser curvature
Lauren classification of gastric adenocarcinoma
- Intestinal type gastric carcinoma
- Typically localized
- Polypoid, glandular formation
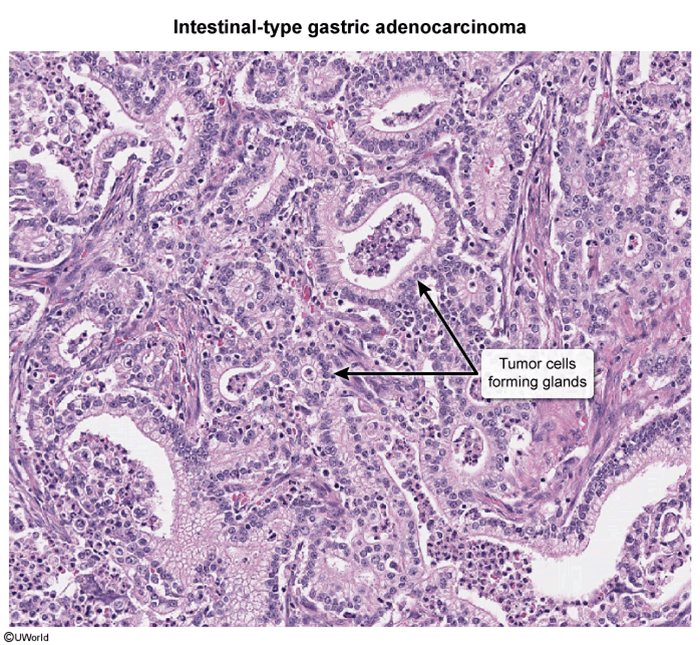
- Similar to an ulcerative lesion with clear raised margins
- Commonly located on the lesser curvature
- Must be differentiated from peptic gastric ulcers by biopsy
- Diffuse type gastric carcinoma
- No clear border
- Spreads earlier in the course of disease
- Infiltrative growth
- Diffuse spread in the gastric wall
- Linitis plastica: gastric wall thickening and leather bottle appearance
- Composed of signet ring cells: round cells filled with mucin, with a flat nucleus in the cell periphery
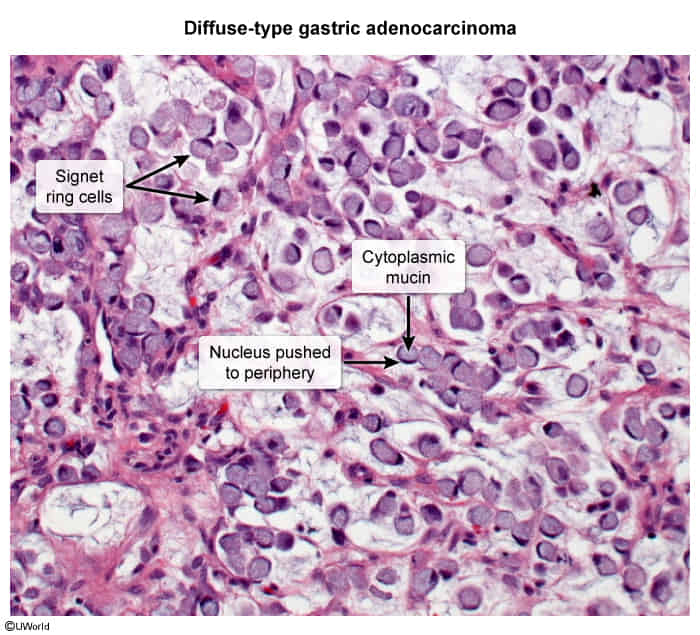
- Associated with E-cadherin mutation
- E-cadherin is a family of calcium-dependent glycoproteins that facilitate cell-to-cell adhesion at adherens junctions. Link to the actin cytoskeleton via catenin and vinculin.
- Due to its role in cell adhesion and differentiation, E-cadherin protects against tumor formation. Low expression is associated with poorer prognosis (e.g., increased depth of invasion or severe lymph node involvement).
Treatment
Complications
Postgastrectomy complications
Dumping syndrome
- Definition: rapid gastric emptying as a result of defective gastric reservoir function, impaired pyloric emptying mechanisms, or anomalous postsurgery gastric motor function
Early dumping
- Pathophysiology: dysfunctional or bypassed pyloric sphincter → rapid emptying of undiluted hyperosmolar chyme into the small intestine → fluid shift to the intestinal lumen → small bowel distention → vagal stimulation → increased intestinal motility
- Clinical features
- Occur within 15–30 minutes after meal ingestion
- Include nausea, vomiting, diarrhea, and cramps
- Vasomotor symptoms such as sweating, flushing, and palpitations
- Management
- Dietary modifications: small meals that include a combination of complex carbohydrates and foods rich in protein and fat
Late dumping
- Pathophysiology: dysfunctional pyloric sphincter → rapid emptying of glucose-containing chyme into the small intestine → quick reabsorption of glucose → hyperglycemia → excessive release of insulin → hypoglycemia and release of catecholamines
- Clinical features
- Occur hours after meal ingestion
- Include signs of hypoglycemia (e.g., hunger, tremor, lightheadedness)
- GI discomfort
- Management
- Dietary modifications
- Second-line treatment: octreotide
- Third-line treatment: surgery