Mnemonic
Antipsychotics are thought to work by blocking the D2 receptor. Psychotic patients sometimes take a DetouR from reality.
| Characteristic | High-Potency FGAs | Low-Potency FGAs | SGAs (Atypicals) |
|---|---|---|---|
| Examples | Haloperidol, Fluphenazine | Chlorpromazine | Risperidone, Olanzapine, Clozapine |
| EPS Risk | ↑↑↑ (High) | ↓ (Low) | ↓↓↓ (Lowest) |
| Metabolic Risk (Wt Gain, DM) | ↓ (Low) | ↓ (Low) | ↑↑↑ (High) |
| Other SEs (Anticholinergic, Sedation, Hypotension) | ↓ (Low) | ↑↑↑ (High) | Variable |
| Key Clinical Note | Best for acute agitation, but high risk of EPS. | High side effect burden limits use. | First-line for schizophrenia due to lower EPS risk & efficacy for negative Sx. |
| ”Must-Know” SE | Tardive Dyskinesia (TD) | Sedation, Orthostatic Hypotension | Metabolic Syndrome Agranulocytosis (Clozapine) Hyperprolactinemia (Risperidone) |
| Drug Class | Primary Receptor Dynamic | Resulting Clinical Profile |
|---|---|---|
| High-Potency FGA | Tight D2 binding (Specific) | High EPS; minimal off-target effects. |
| Low-Potency FGA | Loose D2 binding + High Dose (Non-specific) | High Anti-HAM side effects (Histamine/Alpha/Muscarinic); Low EPS (due to intrinsic anticholinergic activity). |
| SGA (Atypical) | 5-HT2A Antagonism > D2 Antagonism | Low EPS (5-HT blockade boosts Dopamine in striatum); Metabolic Syndrome (due to H1/5-HT2C effects). |
- First-generation antipsychotics (also called typical antipsychotics)
- Mechanism: Potent D2 receptor antagonists.
- Clinical Use: Primarily treat positive symptoms of schizophrenia (hallucinations, delusions).
- Side Effects: High risk of Extrapyramidal Symptoms (EPS) and hyperprolactinemia.
- High-Potency FGAs
- Drugs: Haloperidol, Fluphenazine (“Try to Fly High”).
- Side Effects: High risk of EPS. Lower risk of anticholinergic, antihistaminic, and anti-alpha-1 side effects.
- Low-Potency FGAs
- Low potency means they bind weakly to D2 receptors. You need a much larger dose to get the same antipsychotic effect. So they also happen to block other receptors.
- Drugs: Chlorpromazine, Thioridazine (“Cheating Thieves are Low”).
- Side Effects: Low risk of EPS. High risk of:
- Anticholinergic (dry mouth, constipation)
- Antihistaminic (sedation)
- Anti-alpha-1 (orthostatic hypotension)
- Second-generation antipsychotics (also called atypical antipsychotics)
- Mechanism: Block D2 and Serotonin (5-HT2A) receptors. t
- Serotonin antagonism can help modulate dopamine, reducing its EPS side effect.
- Clinical Use: First-line for schizophrenia; treat both positive and negative symptoms.
- Side Effects: Lower risk of EPS and tardive dyskinesia compared to FGAs. Major side effects are metabolic.
- Mechanism: Block D2 and Serotonin (5-HT2A) receptors. t
Tip
Antipsychotics block dopamine receptor, instead of inhibiting dopamine reuptake, as seen in antidepressants.
- Dopamine Pathways & Effects of Blockade:
- Mesolimbic: Therapeutic effect (reduces positive symptoms).
- Nigrostriatal: Causes Extrapyramidal Symptoms (EPS).
- Tuberoinfundibular: Causes hyperprolactinemia (e.g., gynecomastia, galactorrhea, amenorrhea).
First-generation antipsychotics (FGAs)
High-potency
Haloperidol
- Brand name: Haldol
- High-potency antipsychotics
- Dopamine-specific antagonism (D2 receptor)
- Extrapyramidal symptoms most common in high-potency FGAs
- HOLD-ol

- HOLD-ol
Adverse effects
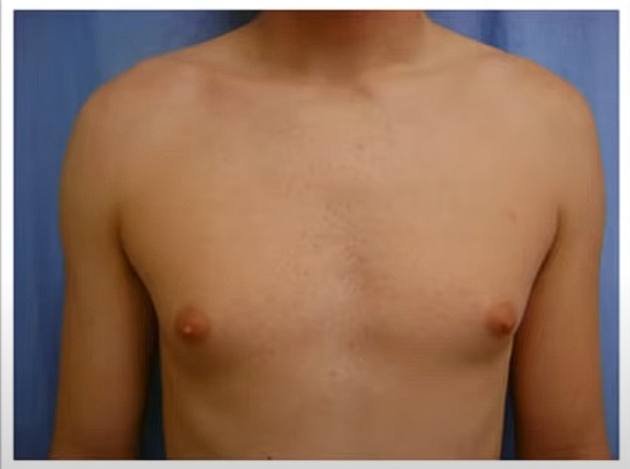
- Hyperprolactinemia
- Dopamine inhibits the release of prolactin via the D2 receptor in the tuberoinfundibular pathway. Therefore, dopamine antagonists increase the effects of prolactin.
- Extrapyramidal symptoms most common in high-potency FGAs
- Prolonged QT interval
- Neuroleptic malignant syndrome
Low-potency
Chlorpromazine
- Low-potency antipsychotics
- Dopamine antagonism
- Anticholinergic
- Antihistaminergic
- First discovered, wide range of indications
- Corneal deposits
Mnemonic
氯丙嗪,治精神;阻断多巴Ma不灵。止吐冬眠和降温,就是不治晕动病。不良反应帕金森,张口伸舌坐不能。口干好似阿托品,乳汁分泌羞死人。
Mnemonic
Chlor-neal deposits
Adverse effects
- Anticholinergic effects, sympatholytic effects, metabolic effects, and sedation dominate
- Sedation due to histamine receptor blockade, see Antihistamines
Difference of Adverse Effects
Low-potency antipsychotics require higher doses to achieve the desired effect, which leads to more prominent blockage of other receptors except D2.
Second-generation antipsychotics (SGAs)
Clozapine
- Most effective antipsychotic
- Indications
- Treatment-resistant schizophrenia
- Schizophrenia associated with suicidality
- Clozapine can cause agranulocytosis and lowers the seizure threshold
Mnemonic
You must watch clozapine clozely to monitor for agranulocytosis!
Olanzapine
- Second effective antipsychotic, without risk of agranulocytosis
- Metabolic effects (usually weight gain, hyperglycemia, new-onset diabetes mellitus, dyslipidemia) most prominent
Mnemonic
Olanzapine can make patients gain weight, so it’s the pharmacological choice for Anorexia nervosa
Risperidone
- Less sedation, good for elderly patients
Mnemonic
Rise and shine
Quetiapine
- More sedation
Mnemonic
Quietiapine
Adverse effects
Summary
- Extrapyramidal side effects:
- Tardive dyskinesia:
- Involuntary movements after chronic use (e.g., lip smacking, choreoathetoid movements)
- Neuroleptic malignant syndrome:
- Fever, rigidity, mental status changes, autonomic instability
- First-generation antipsychotics (FGAs)
- High-potency (eg, haloperidol)
- Extrapyramidal symptoms (acute dystonia, akathisia, parkinsonism), tardive dyskinesia
- Low-potency (eg, chlorpromazine)
- Sedation, cholinergic blockade, orthostatic hypotension, weight gain
- High-potency (eg, haloperidol)
- Second-generation antipsychotics (SGAs)
- Metabolic syndrome, weight gain
- Extrapyramidal symptoms (less common than FGAs)
Hyperprolactinemia
- Elevated prolactin levels: Dopamine inhibits the release of prolactin via the D2 receptor in the tuberoinfundibular pathway. Therefore, dopamine antagonists increase the effects of prolactin.
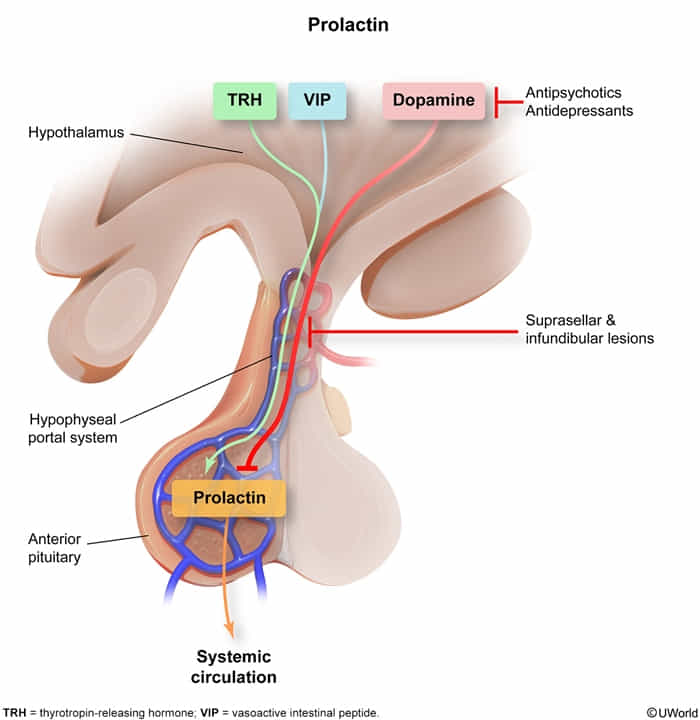
- ↑ Prolactin → suppression of GnRH → ↓ LH, ↓ FSH → ↓ estrogen, ↓ testosterone → hypogonadotropic hypogonadism
- Most common in risperidone, amisulpride
- In men: gynecomastia, galactorrhea, hypogonadotropic hypogonadism (erectile dysfunction, reduced libido, infertility)
- In women: galactorrhea, oligomenorrhea, hypogonadotropic hypogonadism (amenorrhea, reduced libido, infertility)
Mnemonic
RISE-PAIR-idone gives RISE to a PAIR
Extrapyramidal symptoms (EPS)
- Pathophysiology: Inhibition of the nigrostriatal dopaminergic pathways results in EPS.
- First-generation high-potency antipsychotics: D2 antagonism → EPS
- Second-generation antipsychotics: weaker D2 antagonism → fewer EPS
- Clinical features similar to Parkinson disease: Muscle, rustle, and hustle
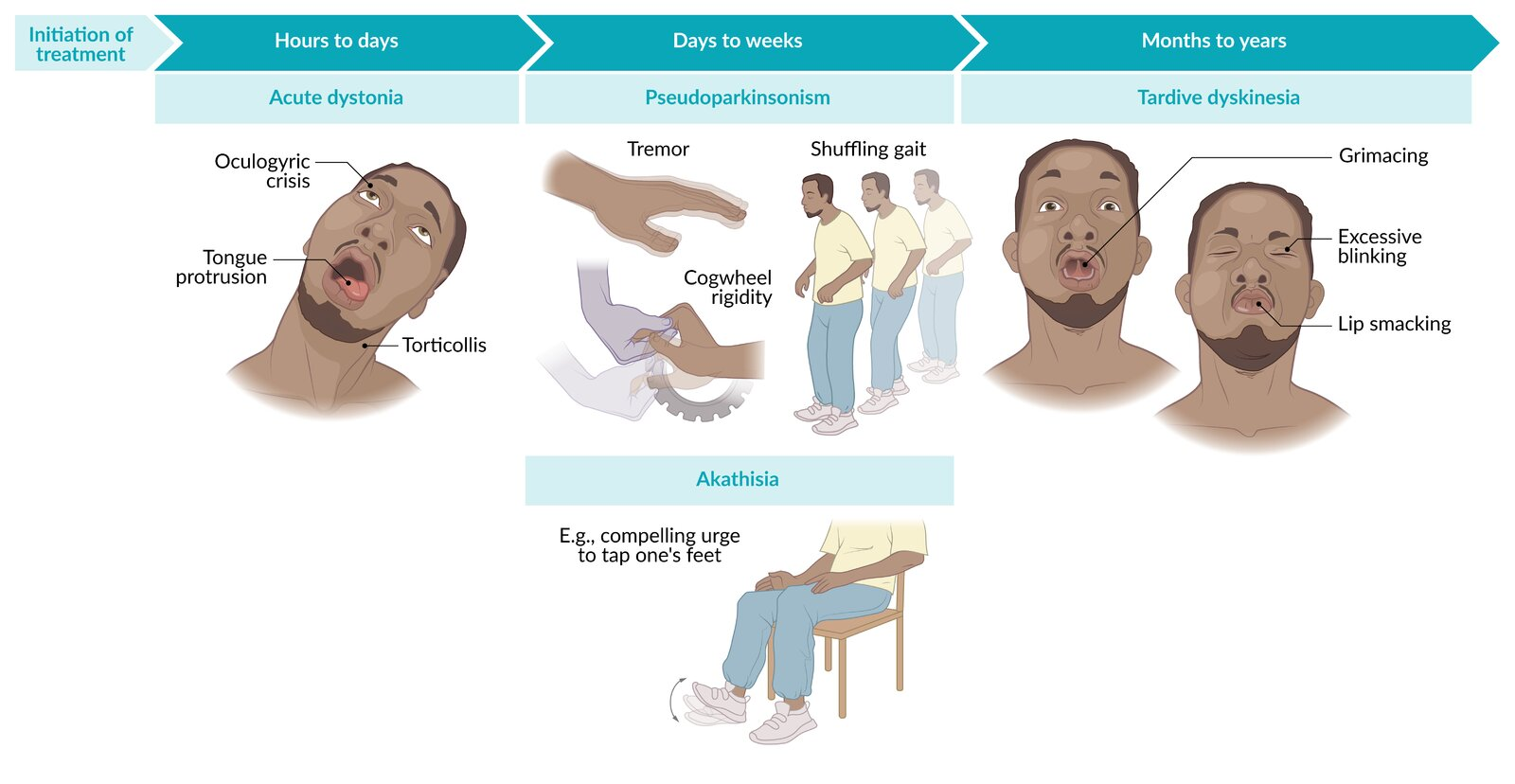
- Acute dystonia
- Onset: Hours to days
- Painful and lasting muscle spasms and stiffness predominantly affecting the head, neck, and tongue
- Facial grimacing, torticollis
- Tongue protrusion or twisting
- Oculogyric crisis (upward deviation of the eyes)
- In severe cases: laryngospasm, opisthotonus of the back
- Pseudoparkinsonism
- Onset: ∼ 1–4 weeks
- Akathisia
- 1–8 weeks
- Restlessness/compelling urge to move
- Inability to sit or stand still
- See Restless legs syndrome
- Tardive dyskinesia
- Months to years
- Pathophysiology: Long-term D2 receptor blockade leads to upregulation and supersensitivity of postsynaptic dopamine receptors.
- Repetitive chewing and lip smacking
- Choreic movements
- Can be irreversible if drug is not discontinued
- Acute dystonia
- Treatment
- Decrease or discontinue offending medication
- Anticholinergics (trihexyphenidyl, benztropine)
Mnemonic
Chewing Tardive
Neuroleptic malignant syndrome
Tip
Malignant Hyperthermia and Neuroleptic Malignant Syndrome (NMS) have almost same symptoms. The only differentiating factor is
- Malignant Hyperthermia is triggered by inhaled anesthetics (e.g., halothane) or succinylcholine
- NMS is triggered by antipsychotics
Epidemiology
Etiology
- High-potency first-generation antipsychotics (most common association)
- Second-generation antipsychotics
- Other dopamine antagonists, e.g., metoclopramide, promethazine
Pathophysiology
- Central D2 receptor blockade in the nigrostriatal pathway and hypothalamus, resulting in movement disorders and impaired thermoregulation
Clinical features
- Mental status changes (encephalopathy)
- Delirium (e.g., reduced vigilance)
- Confusion
- Stupor
- Catatonia
- Parkinsonism
- Hyperthermia: High-grade fever is common.
- Because muscles working overtime
- Autonomic instability
- Tachycardia, dysrhythmias, labile blood pressure
- Tachypnea
- Diaphoresis
Diagnostics
Clinical features similar to Serotonin syndrome
Neuroleptic malignant syndrome Serotonin syndrome Precipitant Dopamine antagonist Serotonergic agent Onset 1-3 days <1 day Altered mental status Yes Yes Sympathetic hyperactivity Yes Yes Diffuse rigidity ”Lead-pipe” rigidity No Clonus No Yes Reflexes Hyporeflexia Hyperreflexia
Tip
- Neurotransmitter Specificity:
- Dopamine Blockade in NMS:
- Dopamine is crucial for inhibiting overactivity in muscle movements. Its blockade removes this inhibition, causing muscles to become rigid.
- The lack of dopamine dampens reflex arcs, leading to hyporeflexia.
- Serotonin Excess in Serotonin Syndrome:
- Serotonin enhances excitatory signals in the nervous system.
- Increased serotonin amplifies reflex pathways, resulting in hyperreflexia and clonus.
- Neuromuscular Impact:
- The balance between inhibitory and excitatory neurotransmitters is essential for normal muscle function.
- NMS tips the scale towards inhibition loss (due to dopamine blockade), causing rigidity.
- Serotonin syndrome tips the scale towards excess excitation, leading to clonus and hyperactive reflexes.
Treatment
- Discontinue suspected causative agent (e.g., antipsychotics).
- Pharmacotherapy
- Skeletal muscle relaxant: Dantrolene (See Treatment)
- Dopamine agonists, e.g., bromocriptine, amantadine, or apomorphine
- Benzodiazepines, e.g., lorazepam: can be used to treat mild symptoms of NMS and/or psychomotor agitation
- Calcium-channel blockers: for hypertension
Link to original
Neuroleptic malignant syndrome
Tip
Malignant Hyperthermia and Neuroleptic Malignant Syndrome (NMS) have almost same symptoms. The only differentiating factor is
- Malignant Hyperthermia is triggered by inhaled anesthetics (e.g., halothane) or succinylcholine
- NMS is triggered by antipsychotics
Epidemiology
Etiology
- High-potency first-generation antipsychotics (most common association)
- Second-generation antipsychotics
- Other dopamine antagonists, e.g., metoclopramide, promethazine
Pathophysiology
- Central D2 receptor blockade in the nigrostriatal pathway and hypothalamus, resulting in movement disorders and impaired thermoregulation
Clinical features
- Mental status changes (encephalopathy)
- Delirium (e.g., reduced vigilance)
- Confusion
- Stupor
- Catatonia
- Parkinsonism
- Hyperthermia: High-grade fever is common.
- Because muscles working overtime
- Autonomic instability
- Tachycardia, dysrhythmias, labile blood pressure
- Tachypnea
- Diaphoresis
Diagnostics
Clinical features similar to Serotonin syndrome
| Neuroleptic malignant syndrome | Serotonin syndrome | |
|---|---|---|
| Precipitant | Dopamine antagonist | Serotonergic agent |
| Onset | 1-3 days | <1 day |
| Altered mental status | Yes | Yes |
| Sympathetic hyperactivity | Yes | Yes |
| Diffuse rigidity | ”Lead-pipe” rigidity | No |
| Clonus | No | Yes |
| Reflexes | Hyporeflexia | Hyperreflexia |
Tip
- Neurotransmitter Specificity:
- Dopamine Blockade in NMS: - Dopamine is crucial for inhibiting overactivity in muscle movements. Its blockade removes this inhibition, causing muscles to become rigid. - The lack of dopamine dampens reflex arcs, leading to hyporeflexia.
- Serotonin Excess in Serotonin Syndrome: - Serotonin enhances excitatory signals in the nervous system. - Increased serotonin amplifies reflex pathways, resulting in hyperreflexia and clonus.
- Neuromuscular Impact:
- The balance between inhibitory and excitatory neurotransmitters is essential for normal muscle function.
- NMS tips the scale towards inhibition loss (due to dopamine blockade), causing rigidity.
- Serotonin syndrome tips the scale towards excess excitation, leading to clonus and hyperactive reflexes.
Treatment
- Discontinue suspected causative agent (e.g., antipsychotics).
- Pharmacotherapy
- Skeletal muscle relaxant: Dantrolene (See Treatment)
- Dopamine agonists, e.g., bromocriptine, amantadine, or apomorphine
- Benzodiazepines, e.g., lorazepam: can be used to treat mild symptoms of NMS and/or psychomotor agitation
- Calcium-channel blockers: for hypertension