Classifications of Interstitial Lung Diseases
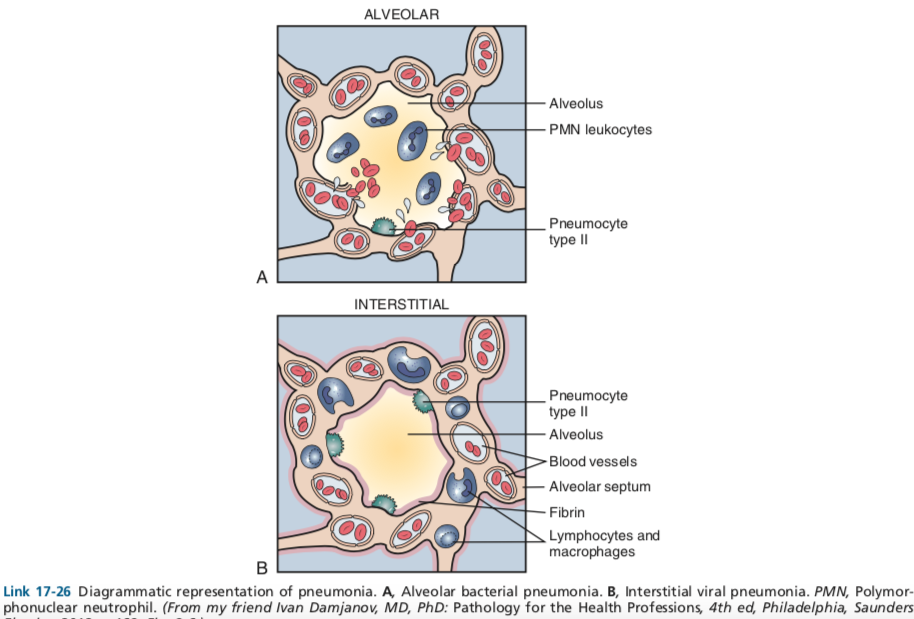
Interstitial Lung Diseases (ILDs) are a heterogeneous group of disorders characterized by inflammation and/or fibrosis of the lung interstitium. Classification is based on etiology and histopathology.
1. ILDs of Known Cause
- Connective Tissue Disease-Associated ILD (CTD-ILD): Lung involvement is a common and serious complication of autoimmune diseases.
- Examples: Systemic Sclerosis (Scleroderma), Rheumatoid Arthritis (RA), Sjögren’s Syndrome, Polymyositis/Dermatomyositis (PM/DM), Systemic Lupus Erythematosus (SLE).
- Key Feature: ILD may be the first manifestation of the underlying CTD.
- Dx: Requires autoimmune serologies (e.g., ANA, anti-Scl-70, RF, anti-CCP, anti-Jo-1).
- Hypersensitivity Pneumonitis (HP): Immune response to inhaled organic antigens.
- Etiology: Exposure to antigens like moldy hay (Farmer’s Lung), bird droppings/feathers (Bird Fancier’s Lung), or contaminated humidifiers.
- Patho: Can be a mix of Type III (immune complex) and Type IV (delayed, T-cell mediated) hypersensitivity reactions.
- Presentation:
- Acute: Flu-like symptoms (fever, cough, dyspnea) 4-8 hours post-exposure.
- Chronic: Progressive dyspnea and fibrosis with long-term, low-level exposure.
- Dx: History of exposure is key. Precipitating IgG antibodies to the offending antigen. HRCT may show ground-glass opacities and poorly formed, non-caseating granulomas.
- Drug-Induced ILD:
- Common culprits: Amiodarone, Bleomycin, Methotrexate, Nitrofurantoin, Radiation therapy.
- Pneumoconioses (Occupational Exposures):
- Asbestosis: Shipbuilding, roofing, plumbing. Affects lower lobes. Associated with pleural plaques and ↑ risk of bronchogenic carcinoma & mesothelioma.
- Silicosis: Mining, sandblasting, quarrying. Affects upper lobes. Associated with “eggshell” calcification of hilar lymph nodes and ↑ risk of TB.
- Berylliosis: Aerospace, manufacturing. Mimics sarcoidosis with non-caseating granulomas.
- Coal Worker’s Pneumoconiosis: Coal mining. Affects upper lobes.
2. Idiopathic Interstitial Pneumonias (IIPs)
This is a group of ILDs with no known cause, classified by specific histopathologic patterns.
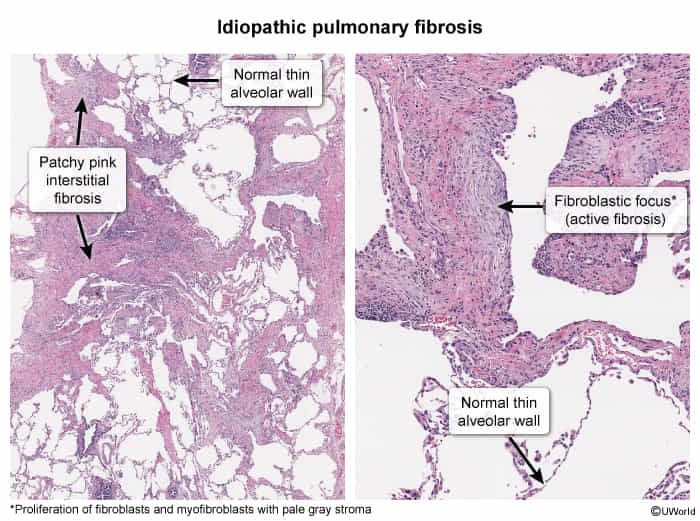
- Idiopathic Pulmonary Fibrosis (IPF)
- Pathophysiology/Etiology
- Chronic, progressive, fibrosing interstitial pneumonia of unknown cause.
- Believed to result from recurrent alveolar epithelial cell injury in a susceptible individual, leading to an abnormal wound-healing response with excessive collagen deposition.
- Risk factors: smoking, environmental exposures (metal/wood dust), certain viral infections, and genetic predisposition (e.g., telomerase mutations).
- Clinical Presentation
- Insidious onset of progressive exertional dyspnea and a persistent non-productive cough, typically in males > 60 years old.
- Physical exam: Fine “Velcro-like” inspiratory crackles at the lung bases are characteristic. Digital clubbing is seen in ~50% of patients.
- Systemic symptoms like fatigue and weight loss can occur but are less common.
- Diagnosis
- Requires exclusion of other causes of interstitial lung disease (e.g., connective tissue disease, drug toxicity, hypersensitivity pneumonitis).
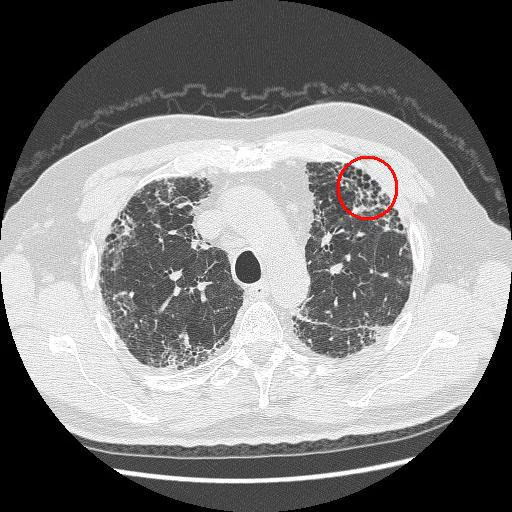
- High-Resolution CT (HRCT) of the chest is the key imaging modality.
- Typical Usual Interstitial Pneumonia (UIP) pattern on HRCT is diagnostic and includes:
- Subpleural, basilar predominant reticulation.
- Honeycombing (clustered cystic airspaces), with or without traction bronchiectasis.
- Typical Usual Interstitial Pneumonia (UIP) pattern on HRCT is diagnostic and includes:
- Pulmonary Function Tests (PFTs): Show a restrictive pattern (↓ FVC, ↓ TLC, normal or ↑ FEV1/FVC ratio) and impaired gas exchange (↓ DLCO).
- Surgical lung biopsy is the gold standard if HRCT is not definitive, showing a histologic UIP pattern (patchy fibrosis, fibroblastic foci).
- Pathophysiology/Etiology
- Cryptogenic Organizing Pneumonia (COP)
- Patho/Etiology
- Idiopathic, non-infectious pneumonia characterized by intra-alveolar buds of granulation tissue (Masson bodies) in distal airways, alveolar ducts, and alveoli.
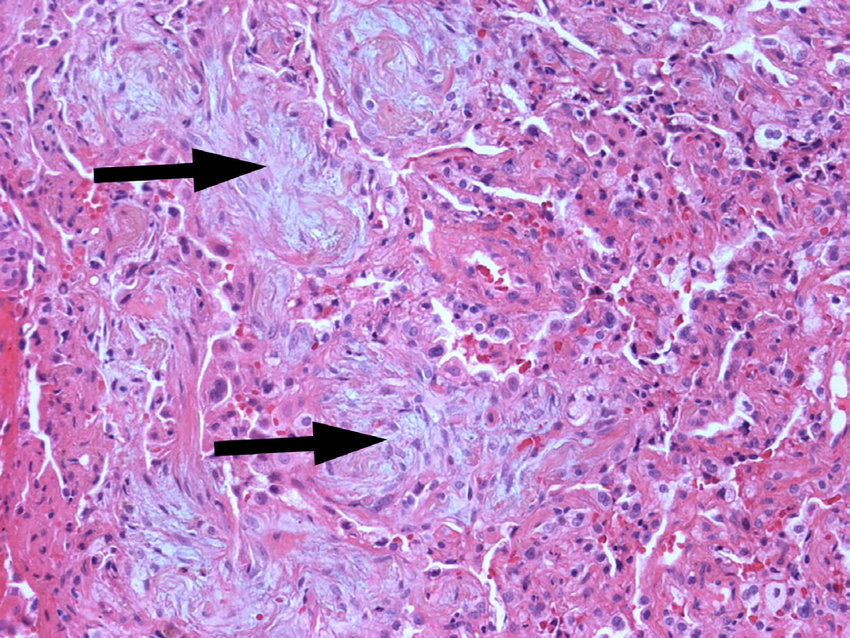
- Represents a nonspecific response to alveolar epithelial injury. The underlying lung architecture is preserved.
- “Cryptogenic” implies no known cause. Organizing pneumonia (OP) can be secondary to infections, drugs (e.g., amiodarone), connective tissue diseases (e.g., RA, polymyositis), or radiation.
- Idiopathic, non-infectious pneumonia characterized by intra-alveolar buds of granulation tissue (Masson bodies) in distal airways, alveolar ducts, and alveoli.
- Clinical Presentation
- Typically affects patients in their 50s-60s.
- Subacute onset (weeks to months) of a flu-like illness that fails to respond to antibiotics.
- Key symptoms: persistent non-productive cough, dyspnea, fever, malaise, weight loss.
- Physical exam: inspiratory crackles (“Velcro rales”) are common. Clubbing is characteristically absent.
- Diagnosis
- CXR: Bilateral, patchy, peripheral alveolar opacities. Opacities can be migratory.
- HRCT (High-Resolution CT): Gold standard for imaging. Shows patchy airspace consolidation, ground-glass opacities, and nodules, often with a peripheral/subpleural or peribronchial distribution.
- “Reversed halo sign” or “Atoll sign” (central ground-glass opacity surrounded by a denser rim of consolidation) is highly specific but not very sensitive.
- PFTs: Usually show a restrictive pattern.
- Bronchoalveolar Lavage (BAL): Shows a mixed inflammatory pattern with increased lymphocytes, neutrophils, and eosinophils. Helps to exclude infection.
- Surgical Lung Biopsy (VATS): Gold standard for definitive diagnosis. Histology reveals polypoid plugs of loose organizing connective tissue (Masson bodies) in the alveoli.
- Patho/Etiology
- Smoking-Related ILDs
- Respiratory Bronchiolitis-ILD (RB-ILD) and Desquamative Interstitial Pneumonia (DIP): Both occur almost exclusively in smokers. Characterized by pigment-laden macrophages in respiratory bronchioles (RB-ILD) or alveolar spaces (DIP). Good prognosis with smoking cessation.
3. Granulomatous ILDs
- Sarcoidosis: A multisystem disease of unknown etiology characterized by non-caseating granulomas.
Pathophysiology
- General
- All types of ILDs share the same basic pathophysiology.
- Repeated cycles of tissue injury in the lung parenchyma with aberrant wound healing → collagenous fibrosis → remodeling of the pulmonary interstitium
- Pneumoconiosis: inhalation of dust particles → phagocytosis by alveolar macrophages → destruction of alveolar macrophages, inflammatory reaction → scarring, granuloma formation
Clinical features
Diagnostics
High-resolution CT (HRCT) chest
- Typical UIP pattern findings
- Honeycombing: multiple cystic lesions within the lung parenchyma due to fibrosis

- Irregular thickening of intralobular septa
- Reticular pattern and mild ground glass opacity (GGO)
- Traction bronchiectasis (irreversible dilatation of the bronchi and bronchioles due to fibrosis)
- Honeycombing: multiple cystic lesions within the lung parenchyma due to fibrosis
Pulmonary function tests (PFTs)
- Restrictive lung disease pattern
- ↓ Total lung capacity and ↓ vital capacity
- Normal or ↓ FEV1
- ↓ FVC
- Normal or ↑ FEV1:FVC ratio
- The increased elastic recoil results in increased radial traction (outward pulling) on the airways, leading to increased expiratory flow rates when corrected for the low lung volume.
- Decreased diffusing capacity for CO (DLCO): highly sensitive parameter