Infection in asplenic patients
General Increased risk of fulminant and life-threatening infections and sepsis for up to 30 years or longer after splenectomy
Overwhelming postsplenectomy infection (OPSI) and asplenic sepsis
- Definition: a bacterial infection that rapidly progresses to fulminant, overwhelming sepsis in the setting of anatomic or functional asplenia
- Etiology: encapsulated bacteria (e.g., Streptococcus pneumoniae, Neisseria meningitidis, Haemophilus influenzae)
- No Spleen Here
- Pathophysiology
- Normally, encapsulated pathogens are opsonized with antibodies & C3b and then phagocytosed by specialized macrophages in the spleen.
- Nearly half of the body’s total immunoglobulins are produced by splenic B-lymphocytes. Splenic opsonizing antibody is of particular importance in the clearance of encapsulated species, as the capsule allows them to resist innate phagocytosis.
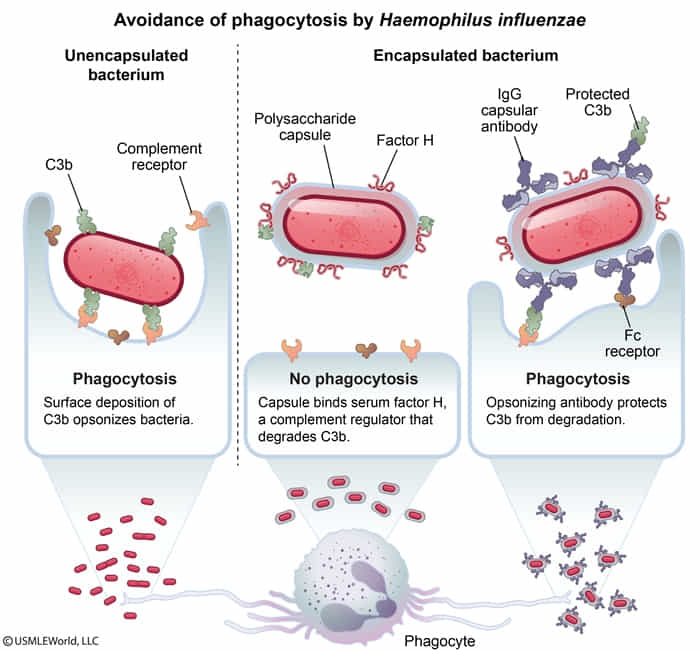
- Nearly half of the body’s total immunoglobulins are produced by splenic B-lymphocytes. Splenic opsonizing antibody is of particular importance in the clearance of encapsulated species, as the capsule allows them to resist innate phagocytosis.
- Individuals with asplenia lack these specialized macrophages, so pathogens are able to spread and cause sepsis.
- Normally, encapsulated pathogens are opsonized with antibodies & C3b and then phagocytosed by specialized macrophages in the spleen.
Tip
People with high susceptibility of encapsulated bacteria:
- Sickle cell anemia
- C3 deficiency
- Clinical features: initially flu-like symptoms, followed by rapid deterioration within hours with fever, severe malaise, signs of sepsis, and meningitis