Etiology
- Risk factors for asthma include:
- Family history of asthma
- Past history of allergies
- Atopic dermatitis
- Low socioeconomic status
- Allergic asthma (extrinsic asthma) vs Nonallergic asthma (intrinsic asthma)
- Allergic asthma (extrinsic asthma)
- Cardinal risk factor: atopy
- Environmental allergens: pollen (seasonal), dust mites, domestic animals, mold spores
- Allergic occupational asthma from exposure to allergens in the workplace (e.g., flour dust)
- Nonallergic asthma (intrinsic asthma)
- Viral respiratory tract infections (one of the most common stimuli, especially in children)
- Cold air
- Physical exertion (laughter, exercise-induced asthma)
- Gastroesophageal reflux disease (GERD): often exists concurrently with asthma
- Chronic sinusitis or rhinitis
- Medication: aspirin/NSAIDS (aspirin-induced asthma), beta blockers
- Stress
- Irritant-induced occupational asthma (e.g., from exposure to solvents, ozone, tobacco or wood smoke, cleaning agents)
- Allergic asthma (extrinsic asthma)
Tip
- Allergic asthma (extrinsic asthma): A type of asthma triggered by allergens (e.g., pollen, dust mites, mold spores, pet allergens). Typically onset in childhood.
- Nonallergic asthma (intrinsic asthma): A type of asthma that typically develops in patients > 40 years of age.
Pathophysiology
Common underlying pathophysiology
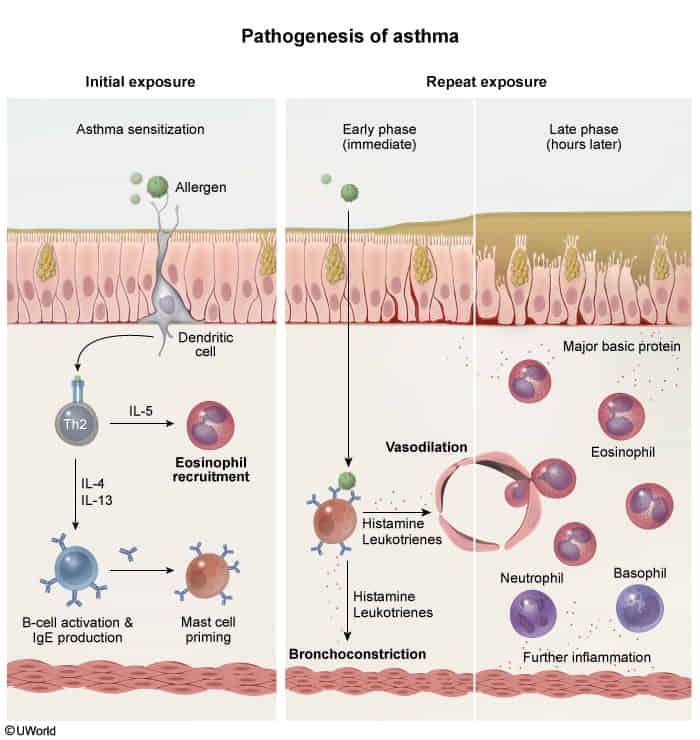
- Core Pathophysiology
- Chronic disorder of airway hyperresponsiveness, inflammation, and reversible bronchoconstriction.
- Symptoms are primarily caused by inflammation of the terminal bronchioles, which are lined with smooth muscle but lack the cartilage found in larger airways.
- Key Cells: Eosinophils, Mast Cells, Th2 lymphocytes.
- Airflow: ↓ FEV1/FVC ratio, reversible with bronchodilators.
- Chronic disorder of airway hyperresponsiveness, inflammation, and reversible bronchoconstriction.
- Allergic (Extrinsic) Asthma
- Type I Hypersensitivity Reaction (most common type).
- Mechanism: Allergen exposure → APC presents to Th2 cell → Th2 secretes:
- IL-4/IL-13: Stimulates B-cells to produce IgE.
- IL-5: Recruits and activates eosinophils.
- Action: IgE coats mast cells. Re-exposure → mast cell degranulation → release of histamine & leukotrienes → bronchospasm.
- Late Phase: Eosinophil-mediated inflammation damages epithelium.
- Non-Allergic (Intrinsic) Asthma
- Triggers: Viral infections (RSV, rhinovirus), cold air, stress.
- Mechanism: Not IgE-mediated. Normal serum IgE. Inflammation is driven by non-atopic stimuli.
- Iirritant enters lung → ↑ release of neutrophils → submucosal edema → airway obstruction
- Aspirin-Exacerbated Respiratory Disease (AERD)
- Samter’s Triad: Asthma + Nasal Polyps + Aspirin/NSAID sensitivity.
- Mechanism: NSAID inhibition of COX pathway shunts arachidonic acid to the lipoxygenase pathway → ↑ Leukotrienes → severe bronchoconstriction.
- Classic Pathology Findings
- Curschmann spirals: Whorled mucus plugs.
- Charcot-Leyden crystals: Crystalline breakdown products of eosinophils.
- Airway Remodeling (Chronic): Smooth muscle hypertrophy and sub-basement membrane fibrosis.
Clinical features
Subtypes and variants
- Allergic asthma
- Most common phenotype
- Begins with intermittent symptoms in childhood
- Triggered by allergens
- Usually associated with atopy (e.g., eczema, rhinitis)
- Responds well to ICS-containing treatment
- Nonallergic asthma
- Less common than allergic asthma
- Triggered by, e.g., viral upper respiratory tract infections, cold air, GERD
- Not associated with atopy
- Responds poorly to ICS-containing treatment
- Cough variant asthma: a type of asthma characterized by chronic dry cough without other typical symptoms of asthma
- Cough often worsens at night.
- Aspirin-exacerbated respiratory disease
- Occupational asthma
Differential diagnostics
| Feature | Cardiogenic “Asthma” (Heart Failure) | Bronchial Asthma |
|---|---|---|
| Pathophysiology | LV failure → pulmonary edema → airway narrowing. | Airway inflammation (IgE/eosinophilic) → bronchoconstriction. |
| Patient Profile | Older patient, history of CHF, HTN, MI. | Younger patient, history of atopy (eczema, allergies). |
| Key Symptoms | Orthopnea, PND, pink frothy sputum. | Nocturnal cough, triggered by allergens/exercise. |
| Physical Exam | JVD, S3 gallop, bibasilar crackles/rales. | Diffuse expiratory wheezing, often normal between exacerbations. |
| Key Diagnostics | ↑ BNP, Kerley B lines & cardiomegaly on CXR. | PFTs show reversible obstruction post-bronchodilator. |
| Management | Diuretics (e.g., Furosemide), Nitrates, O2, BiPAP. | Bronchodilators (e.g., Albuterol), Corticosteroids. |
Diagnostics
Spirometry
- Supportive findings: Expiratory airway limitation: i.e., ↓ FEV1 and ↓ FEV1/FVC ratio
- Bronchodilator Responsiveness Testing:
- Used when the patient has abnormal baseline spirometry showing obstruction (FEV1/FVC ≤70%)
- Tests if the obstruction is reversible (suggesting asthma) or fixed (suggesting conditions like COPD)
- Not useful if current spirometry is normal, even if the patient has asthma symptoms
- Quick test: perform spirometry → give bronchodilator → repeat spirometry
- Bronchial Challenge Testing:
- Identify airway hyperresponsiveness and bronchoconstriction in response to direct, nonallergic stimuli (e.g., methacholine, histamine) or indirect stimuli (e.g., exercise, hyperventilation).
- Used when patient has symptoms suggestive of asthma but normal baseline spirometry
- Tests for airway hyperresponsiveness by attempting to provoke bronchospasm
- Particularly useful for patients with intermittent symptoms who are asymptomatic during office visits
- More time-intensive: involves giving increasing doses of the provocative agent and measuring response
Treatment
Approach
1. Chronic Asthma Management (Stepwise)
- Foundation: Control inflammation with an Inhaled Corticosteroid (ICS). Therapy is stepped up or down based on symptom control.
- Preferred Approach (Single Maintenance and Reliever Therapy - MART):
- Mild (Steps 1-2): As-needed low-dose ICS-formoterol.
- Moderate (Step 3): Daily low-dose ICS-formoterol + as-needed ICS-formoterol for relief.
- Severe (Steps 4-5): Increase to medium/high-dose ICS-formoterol + add-on therapy like a Long-Acting Muscarinic Antagonist (LAMA) or biologics (e.g., anti-IgE, anti-IL-5).
- Key Principle: Pure SABA (e.g., Albuterol) alone is no longer first-line for even mild asthma. An ICS is needed to manage underlying inflammation.
2. Acute Asthma Exacerbation
- Tx (O-SABA-S):
- Oxygen: Maintain SpO2 >92%.
- SABA: High-dose Albuterol (nebulized), often with Ipratropium (a SAMA).
- Systemic Corticosteroids: Oral Prednisone or IV Methylprednisolone are critical to reduce inflammation and prevent relapse.
- Severe/Refractory Tx:
- IV Magnesium Sulfate: For bronchodilation in severe attacks.
- Mechanical Ventilation: If impending respiratory failure (↑PaCO2, ↓mental status, silent chest).

Antileukotrienes
Leukotriene receptor antagonists (LTRAs)
- Montelukast, Zafirlukast
- Uses
- Exercise-induced
- Prevent leukotrienes from binding to their receptors (CysLT1)→ ↓ bronchoconstriction and inflammation
- Asthma aspirin-induced asthma
- Long-term maintenance treatment (particularly in children)
Leukotriene pathway modifiers
- Zileuton
- Inhibit 5-lipoxygenase → ↓ production of leukotrienes → ↓ bronchoconstriction and inflammation
- Uses
- Exercise-induced asthma
- Aspirin-induced asthma
Mnemonic
Antileukotrienes → Montelukast, zafirlukast, zileuton
Long-acting muscarinic antagonists (LAMA)
- Tiotropium bromide(噻托溴铵)
- Long-term maintenance treatment
Mast cell stabilizers (chromones)
- Cromolyn
- Inhibit mast cell degranulation and prevent release of preformed chemical mediators.
- Uses
- Preventive treatment prior to exercise
Biologics
Anti-IgE antibodies
- Omalizumab 单抗记忆
- Binds to serum IgE → ↓ expression of high-affinity IgE receptors (FcεRI) on mast cells and basophils
- Uses
- Select cases of severe asthma
IL-5 antibodies
- mepolizumab, reslizumab,benralizumab
- Block the effects of IL-5 on eosinophils → ↓ chemotaxis and ↓ cell differentiation, maturation, and activation
- Uses
- Refractory severe eosinophilic asthma