Epidemiology
Etiology
- HIV-1
- Epidemiology: Cause of the vast majority (>95%) of HIV infections globally. Responsible for the AIDS pandemic.
- Virulence: More virulent; faster progression to AIDS and higher viral loads.
- Transmission: More easily transmitted than HIV-2.
- HIV-2
- Epidemiology: Primarily concentrated in West Africa.
- Virulence: Less virulent; slower disease progression and lower viral loads.
- Transmission: Less efficiently transmitted.
- Treatment Consideration: Intrinsically resistant to Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs).
- Viral Tropism (Coreceptor Usage for Entry)
- To enter a host cell, HIV must bind to CD4 and a coreceptor. The coreceptor used determines the tropism.
- R5-Tropic (Macrophage-tropic)
- Uses the CCR5 coreceptor.
- Found on macrophages and T-helper cells.
- This is the dominant viral type during initial infection and the asymptomatic phase.
- Targeted by the drug Maraviroc, a CCR5 antagonist. A tropism assay is required before starting this medication.
- X4-Tropic (T-cell-tropic)
- Uses the CXCR4 coreceptor.
- Found primarily on T-helper cells.
- This variant tends to emerge in later stages of the disease.
- Appearance of X4-tropic virus is associated with a more rapid decline in CD4+ cells and faster progression to AIDS.
Pathophysiology
- Key Genes:
env: Glycoproteins gp120 (for host CD4 receptor binding) & gp41 (for fusion and entry).gag: Capsid protein p24.pol: Reverse transcriptase, integrase, protease.- HIV pol gene mutations are responsible for acquired resistance to treatment. Mutations of the env gene enable escape from host-neutralizing antibodies.
Natural history of HIV infection
- HIV infects CD4+ T-helper cells, macrophages, and dendritic cells.
- gp120 binds to CD4 on T-cell.
- gp120 then binds to a coreceptor: CCR5 (early infection, macrophages) or CXCR4 (late infection, T-cells).
- gp41 mediates fusion with the host cell membrane.
- Viral RNA is reverse transcribed into DNA by reverse transcriptase.
- Viral DNA is integrated into the host genome by integrase.
- Host machinery is used to produce viral proteins, which are cleaved by protease to form mature virions.
Clinical features
Acute HIV infection
- Also referred to as acute retroviral syndrome (ARS) or described as a mononucleosis-like syndrome
- Fever
- Fatigue
- Myalgia and arthralgia
- Headache
- Generalized nontender lymphadenopathy
- Generalized rash
- Gastrointestinal symptoms (nausea, diarrhea, weight loss)
- Oropharyngeal symptoms (sore throat, ulcerations, painful swallowing)
Tip
Acute retroviral syndrome is associated with extremely high levels of viral replication (~5 million copies/mL) as the cell-mediated and humoral antibody response against the virus is not yet fully activated. Therefore, laboratory results during this period usually show evidence of HIV in the plasma (positive viral load and p24 antigen) with a negative serologic response (negative HIV-1/HIV-2 antibody). This is referred to as the “window period,” as patients are infected with HIV but HIV antibody screening tests may be negative (newer screening tests incorporate testing for HIV p24 antigen and are more sensitive in early infection).
HIV-associated conditions
AIDS-defining conditions
CD4+ cell count < 500/mm3
- Kaposi sarcoma (typically occurs at CD4 count < 500)
- Lymphoma
- Mycobacterium tuberculosis
CD4+ cell count < 200/mm3
- Pneumocystis pneumonia
- Disseminated or extrapulmonary histoplasmosis
- Progressive multifocal leukoencephalopathy
CD4+ cell count < 100/mm3
- Cerebral toxoplasmosis
- Extrapulmonary cryptococcosis (especially cryptococcal meningitis)
- Cryptosporidiosis
- Etiology: Cryptosporidium species
- Clinical features: chronic, watery diarrhea (lasting > 1 month) with nausea and abdominal pains; typically at CD4 counts < 100
- Diagnostics: acid-fast oocysts in stool
- Esophageal candidiasis or pulmonary candidiasis
- Oropharyngeal candida, which is not AIDS-defining, is more common as CD4 counts decline, and may be seen when CD4 count is < 200–250.
- Neutrophils are the most important immune cell in the defense against invasive Candida infection; therefore, patients with neutropenia (eg, following cytotoxic chemotherapy) are at high risk for invasive disease (eg, candidemia, meningitis). In contrast, T lymphocytes are more important for prevention of superficial, mucocutaneous infection (eg, thrush).
- Primary CNS lymphoma
- Disseminated and/or extrapulmonary Mycobacterium avium complex
- Cytomegalovirus infection
CD4+ cell count < 50/mm3
- Disseminated and/or extrapulmonary Mycobacterium avium complex
- Cytomegalovirus infection
- Aspergillosis
- Primary CNS Lymphoma (PCNSL)
Neurological complications
HIV-associated neurocognitive disorder (HAND)
Link to original
- Definition: neurocognitive impairment in patients with HIV that cannot be attributed to a cause other than HIV infection. HAND is typically a diagnosis of exclusion.
- Etiology: thought to result from a combination of dissemination of HIV into the CNS and the resultant immune activation.
- Epidemiology: common even in patients with well-controlled HIV (affecting up to 50% of individuals)
- Clinical features
- Early: mild impairment in attention, recall, and executive function
- Advanced: HIV-associated dementia (considered an AIDS-defining condition)
- Subcortical dementia: memory loss, depression, movement disorders, behavioral changes (e.g., apathy)
- Severe neurologic deficits: altered mental state, aphasia, gait disturbances
- More common in patients with advanced or untreated HIV
- Diagnostics
- Imaging: CT or MRI brain without and with IV contrast
- Diffuse cerebral atrophy; disproportionate to the patient’s age
- Patchy symmetrical changes in the periventricular and deep white matter
- No mass effect, no contrast-enhancement
- Histopathology shows giant cells with multiple nuclei (formed through fusion of HIV-infected monocytes).
Diagnostics
Serological assays
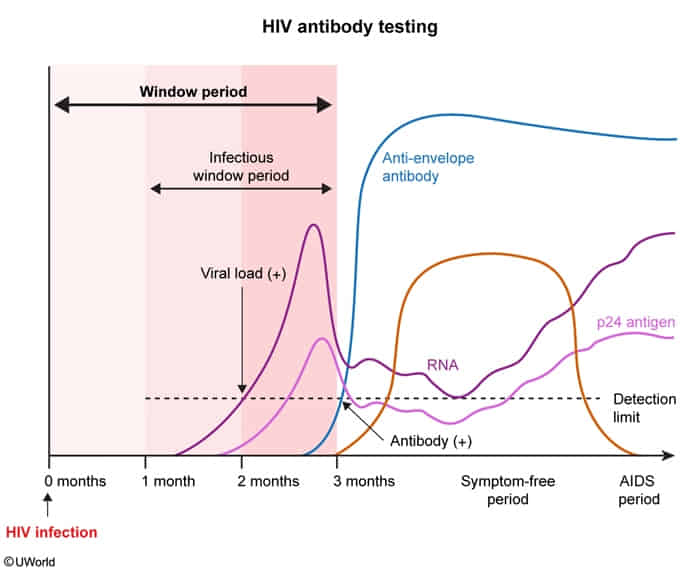
- HIV antibody assays (i.e., third-generation and below): Detect IgM and IgG antibodies.
- Laboratory methods
- Enzyme-linked immunosorbent assays (ELISA)
- HIV-1 and HIV-2 antibody differentiation immunoassay
- Laboratory-based test that can differentiate between HIV-1 and HIV-2 (provides separate results for each analyte)
- Most commonly used confirmatory test in the US
- Western blot: Detects only IgG antibody to HIV-1
- Laboratory methods
- Combination HIV antibody with HIV antigen test (i.e., fourth-generation and above): Can detect HIV IgG and IgM antibodies and p24 antigen.
- Cannot differentiate between HIV-1 and HIV-2 infection
Treatment
See HIV therapy
HIV in pregnancy
- The transmission risk depends on maternal viral load.
- Combined antiretroviral therapy (cART) is recommended throughout pregnancy and delivery. See ART regimens
- In untreated individuals, rates of vertical transmission are as high as 30%. Effective maternal cART and neonatal zidovudine therapy can reduce the risk of perinatal HIV transmission to < 2%.