Etiology
Intrinsic acute kidney injury
Intrinsic causes include any condition that leads to severe direct kidney damage (∼ 35% of cases of AKI).
Info
ATI is an umbrella term indicating a sudden decrease in kidney function. GN, ATN, and ATIN are all causes of ATI.
- Acute tubular necrosis (causes ∼ 85% of intrinsic AKIs)
- Ischemia: e.g., due to prolonged hypotension
- Nephrotoxic drugs: e.g., radiographic contrast agents, aminoglycosides, cisplatin, methotrexate, ethylene glycol, amphotericin B
- Endogenous toxins: e.g., hemoglobin in intravascular hemolysis, myoglobin in rhabdomyolysis, uric acid in TLS, Bence-Jones protein light chains in multiple myeloma
- Acute interstitial nephritis
- Medication: e.g., antibiotics , phenytoin, interferon, PPIs, NSAIDs, cyclosporine
- Infection
- Bacterial: e.g., Legionella spp., Streptococcus spp.
- Fungi: Candida, Histoplasma
- Viral: e.g., hepatitis C virus, cytomegalovirus, HIV
- Infiltrative diseases: e.g., sarcoidosis, amyloidosis
- Vascular diseases
- Hemolytic uremic syndrome (HUS)
- Thrombotic thrombocytopenic purpura (TTP)
- Hypertensive emergency
- Vasculitis, scleroderma renal crisis
- Renal vein thromboses, renal atheroemboli, renal infarction
- Glomerulonephritis:e.g., rapidly progressive glomerulonephritis
Pathophysiology
Prerenal
- Decreased blood supply to kidneys (due to hypovolemia, hypotension, or renal vasoconstriction) → failure of renal vascular autoregulation to maintain renal perfusion → decreased GFR → activation of renin-angiotensin system → increased aldosterone release → increased reabsorption of Na+, H2O → increased Urine osmolality → secretion of antidiuretic hormone → increased reabsorption of H2O and urea
- Creatinine is still secreted in the proximal tubules, so the blood BUN:creatinine ratio increases.
Intrinsic
- Acute Tubular Necrosis (ATN) is the most common cause of intrinsic (renal) acute kidney injury (AKI), especially in hospitalized patients.
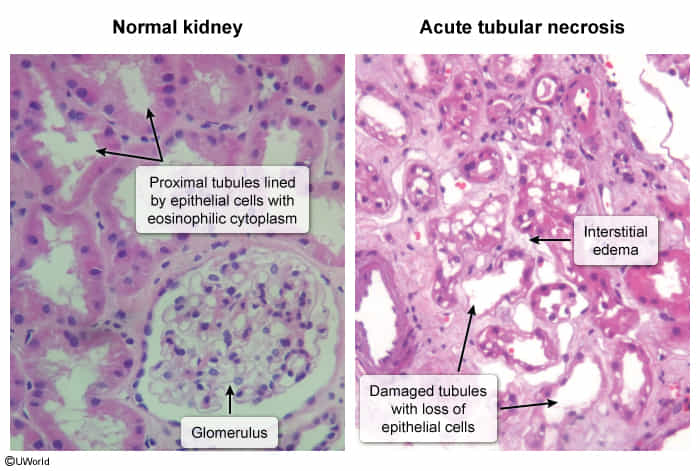
- Characterized by damage and necrosis of renal tubular epithelial cells, primarily affecting the proximal convoluted tubule and the thick ascending limb.
- Damage leads to sloughing of cells into the tubular lumen, forming casts and causing obstruction, which ↓ GFR.
- Damaged tubules have impaired reabsorptive capacity, leading to filtrate backleak into the interstitium.
- Ischemia or toxins also trigger intrarenal vasoconstriction, further reducing renal blood flow.
Postrenal
Four phases of AKI
- Initiating event (kidney injury) (Duration: Hours to days)
- Symptoms of the underlying illness causing AKI may be present.
- Oliguric or anuric phase (maintenance phase) (Duration: 1-3 weeks)
- Progressive deterioration of kidney function
- Reduced urine production (oliguria), < 50 ml/24 hrs = anuria
- Increased retention of urea and creatinine (azotemia)
- Complications: fluid retention (pulmonary edema), hyperkalemia, metabolic acidosis, uremia, lethargy, asterixis
- Progressive deterioration of kidney function
- Polyuric/diuretic phase (Duration: ~ 2 weeks)
- Glomerular filtration returns to normal, which increases urine production (polyuria), while tubular reabsorption remains disturbed.
- Complications: loss of electrolytes and water (dehydration, hyponatremia, and hypokalemia)
- Recovery phase (Duration: Months to years)
- Kidney function and urine production normalize.
Clinical features
Subtypes and variants
Acute tubular necrosis
- Epidemiology: causes ∼ 85% of intrinsic AKIs
- Location (Proximal tubule is most common for both etiologies)
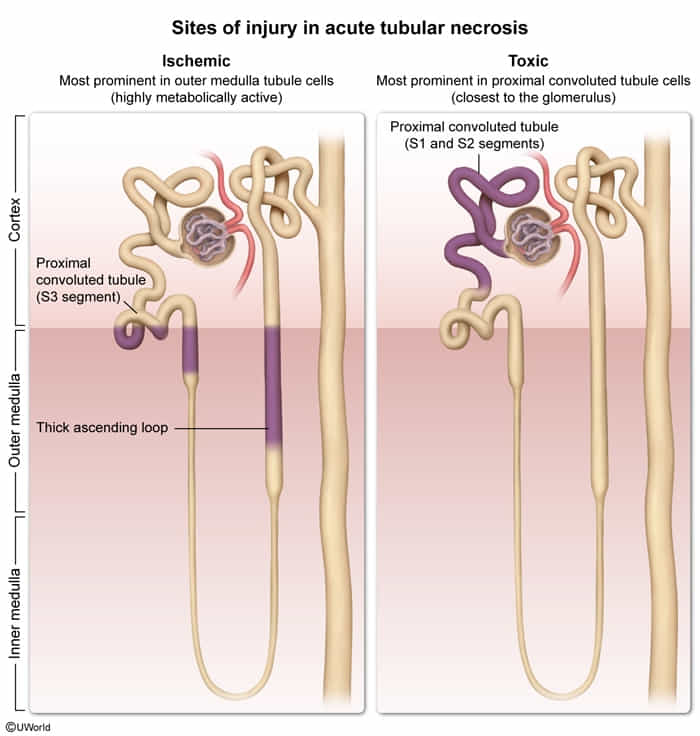
- The straight segment of the proximal tubule and the straight segment of the distal tubule (i.e., the thick ascending limb) are particularly susceptible to ischemic damage.
- Blood flow in the renal medulla is relatively low compared to that in the renal cortex.
- Facilitates the development of an osmolality gradient that allows for effective urine concentration
- Causes medullary vulnerability to hypoxia when renal blood flow is decreased (renal ischemia)
- Blood flow in the renal medulla is relatively low compared to that in the renal cortex.
- The convoluted segment of the proximal tubule is particularly susceptible to damage from toxins (but can also damage from ischemia).
- First encounters toxins
- Descending and ascending limbs are not, as their function is primarily passive.
- The straight segment of the proximal tubule and the straight segment of the distal tubule (i.e., the thick ascending limb) are particularly susceptible to ischemic damage.
- Etiology
- Ischemic: Injury occurs secondary to decreased renal blood flow.
- Severe hypotension, especially in the context of shock: hypovolemic (e.g., hemorrhage, severe dehydration), septic, cardiogenic (e.g., heart failure), or neurogenic shock
- Cholesterol embolism (atheroemboli)
- Toxic: Injury occurs directly due to nephrotoxic substances.
- Contrast-induced nephropathy
- Medication: aminoglycosides, cisplatin, amphotericin, lead, ethylene glycol t
- Pigment nephropathy
- Myoglobinuria due to rhabdomyolysis (crush syndrome)
- Hemoglobinuria associated with hemolysis
- Ischemic: Injury occurs secondary to decreased renal blood flow.
- Pathophysiology: necrotic proximal tubular cells fall into the tubular lumen → debris obstructs tubules → decreased GFR → sequence of pathophysiological events similar to prerenal failure
- Diagnostic
Acute tubular necrosis vs Renal papillary necrosis
- ATN: Oliguria
- Causes: ischemic or toxic
- RPN: Flank pain, hematuria
- Causes: sickle cell disease, NSAIDs
Diagnostics
Urine sediment
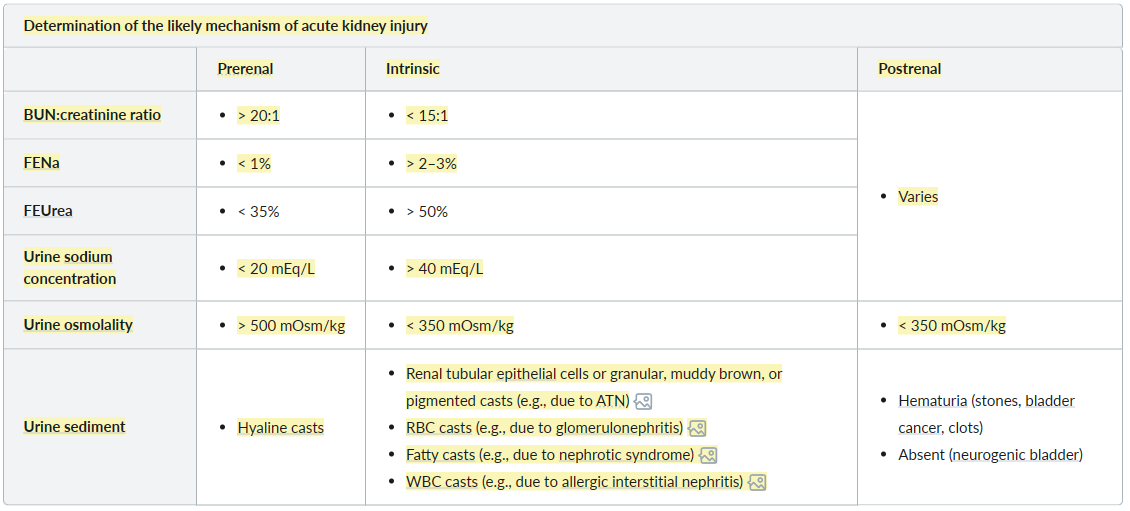
- Prerenal: hyaline casts due to concentrated urine in the setting of low renal perfusion
- Intrinsic: renal tubular epithelial cells or granular, muddy brown, or pigmented casts
- Postrenal: none
| Feature | Acute Tubular Necrosis (ATN) | Acute Tubulointerstitial Nephritis (AIN) | Renal Papillary Necrosis (RPN) |
|---|---|---|---|
| Core Problem | Tubular cell death (ischemia/toxins) | Allergic/inflammatory reaction in interstitium & tubules | Necrosis of renal papillae |
| Key Causes | Shock, Sepsis, Aminoglycosides, Contrast, Myoglobin | Drugs (NSAIDs, Penicillins, PPIs, Sulfa), Infections | NSAIDs, Sickle Cell, Diabetes, Pyelonephritis, Obstruction |
| Classic Presentation | AKI after hypotension or nephrotoxin exposure | Fever, Rash, Arthralgia (triad often absent), AKI after new drug | Hematuria, Flank Pain (especially w/ risk factors) |
| Urinalysis Hallmark | Muddy Brown Granular Casts, RTECs | WBC Casts, Eosinophiluria, Sterile Pyuria | Hematuria, Pyuria, Sloughed Papillae (rarely seen) |
| Key Lab/Diagnostic | FeNa >2%, Urine Osmolality <350 mOsm/kg | Peripheral Eosinophilia | Imaging (CT/IVP): Ring Shadow, Clubbed Calyces |
| Histology Buzzword | Proximal tubule damage, loss of brush border | Interstitial Infiltrate with Eosinophils, Tubulitis | Coagulative Necrosis of Papillae |
| Primary Treatment | Supportive, Remove Toxin, Fluids, Dialysis if severe | Stop Offending Agent, Corticosteroids may be used | Manage Underlying Cause, Supportive, Relieve Obstruction (if any) |