Class I antiarrhythmics
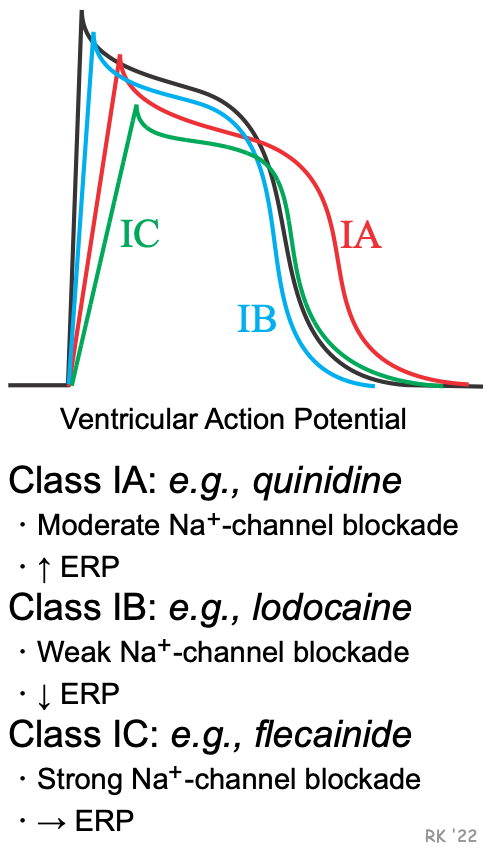 The key here is to separate the effects of sodium channels and potassium channels.
The key here is to separate the effects of sodium channels and potassium channels.
- Sodium channel blockage = slow depolarization + wide QRS + long QT
- Potassium channel blockage = prolonged APD + prolonged ERP. Both of these blocking effects can treat rapid cardiac arrhythmias. Class IA is 1+2, Class IC is only 1 (strongly). However, Class IB is different from the first two as it promotes potassium outflow, thus shortening APD and ERP and increasing ERP:APD ratio
Class III antiarrhythmics
Amiodarone
Tip
Amiodarone has both Class I, II, III & IV actions!
Pharmacodynamics
- Primary mechanism of action: antiarrhythmic effect via blockage of voltage-gated potassium channels → prolonged repolarization of the cardiac action potential
- Secondary mechanism of action: inhibits β-receptors and sodium and calcium channels → decreases conduction through the AV and sinus node
- Special uses: only antiarrhythmic agent with (almost) no negative inotropic effect → use in patients with reduced EF
Other antiarrhythmic drugs
Adenosine
- Mechanism of action: activates Gi protein → inhibition of adenylate cyclase → ↓ cAMP → deactivation of L-type Ca2+ channels and activation of K+ channels → ↓ Ca2+ and ↑ K+ efflux → hyperpolarization → transient AV node block (short-acting, ∼ 15 seconds) → acute termination of supraventricular tachycardia
- Vasodilator
- Coronary autoregulation is a process that maintains myocardial blood flow in settings of decreased coronary perfusion pressure (eg, hemorrhage, sepsis). Within the region of autoregulation (eg, 60-140 mm Hg), changes in coronary blood flow are driven primarily by myocardial oxygen demand. This is accomplished mostly by automated alterations in vascular resistance via the release of locally acting mediators, namely adenosine (released from cardiomyocytes as ATP is broken down for energy) and nitric oxide (synthesized by endothelial cells in response to chemical mediators and mechanical stress).
- When myocardial perfusion pressure decreases, there is decreased oxygen delivery to the myocardium and less ATP is regenerated via oxidative metabolism, resulting in increased levels of adenosine. Myocardial hypoxia also triggers increased synthesis of nitric oxide.
- Indications
- Adverse effects
- Chest pain, flushing, hypotension, bronchospasm
- Sense of impending doom
- AV block, asystole