Epidemiology
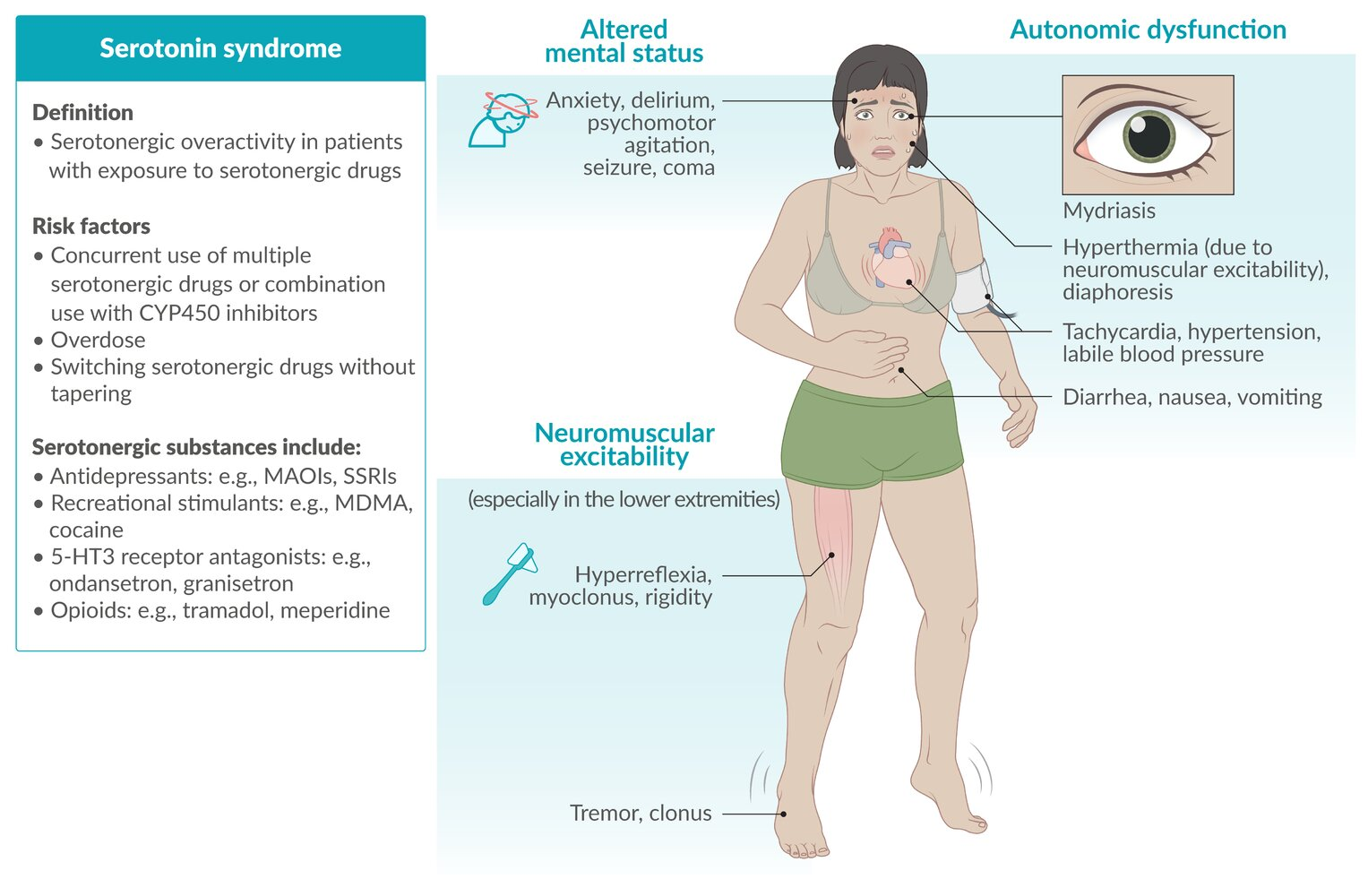
Etiology
Serotonergic drugs
- Antidepressants (e.g., MAOIs, SSRIs, SNRIs, tricyclic antidepressants, vortioxetine, vilazodone, trazodone)
- Anxiolytics (e.g., buspirone)
- Anticonvulsants (e.g., valproate)
- Opioids (e.g., tramadol, meperidine)
- NMDA receptor antagonists (e.g., dextromethorphan)
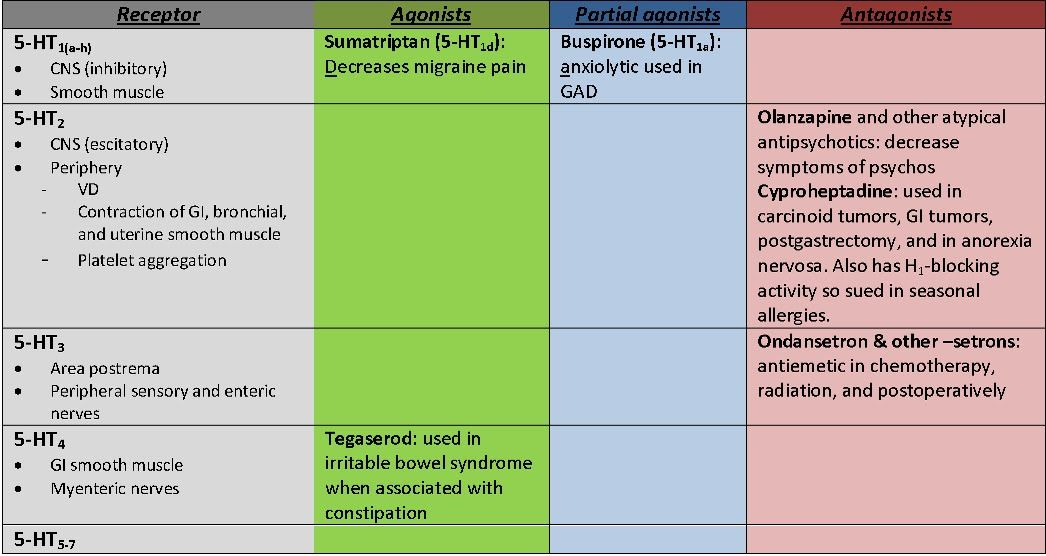
- 5-HT3 receptor antagonists (e.g., ondansetron)
- Serotonin receptor agonists (e.g., triptans, ritonavir)
- Antibiotics (e.g., linezolid)
- Herbal supplements (e.g., St. John’s wort, ginseng, tryptophan)
- Tryptophan is precursor of serotonin
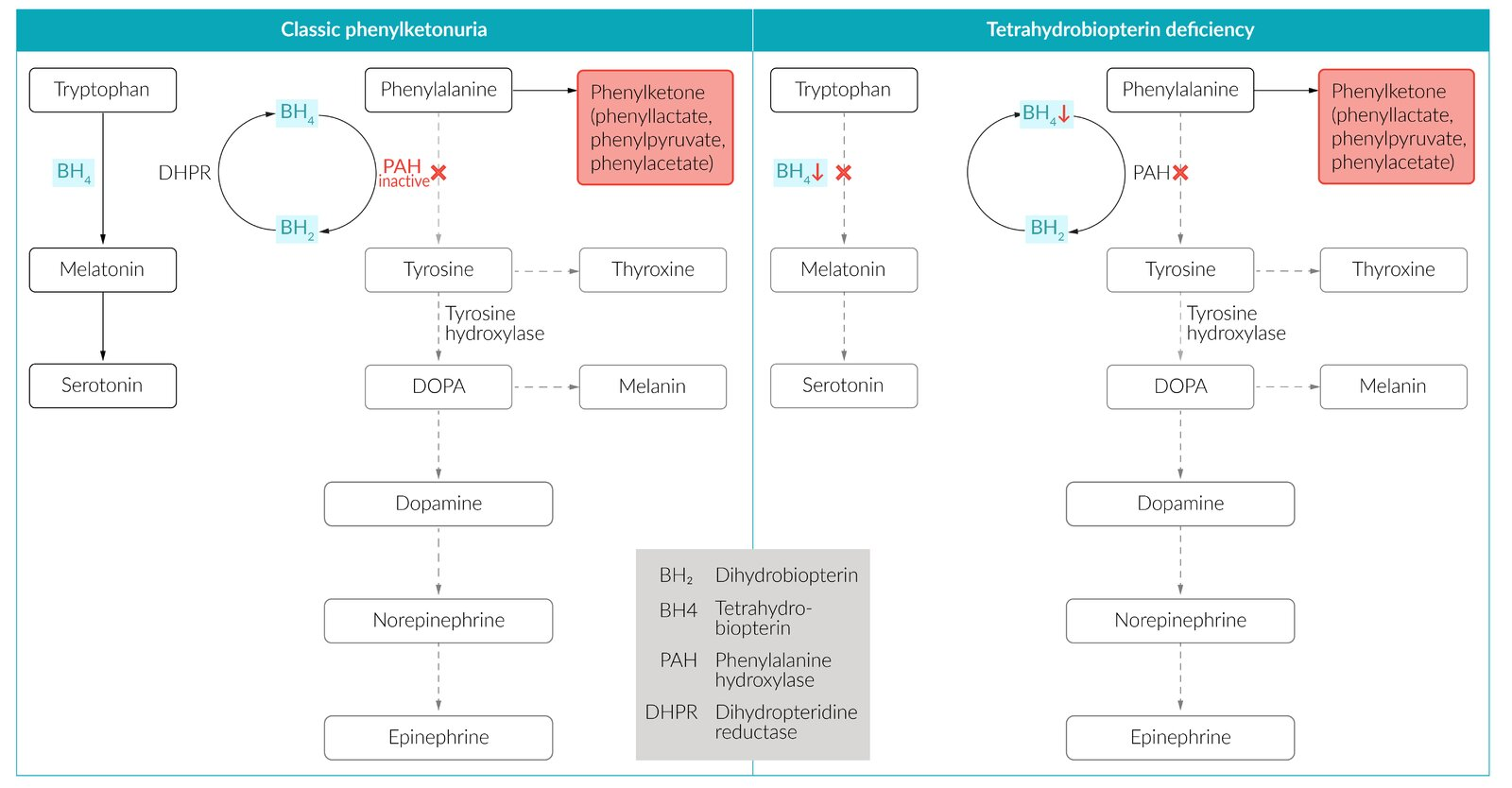
- Tryptophan is precursor of serotonin
- Recreational stimulants (e.g., MDMA, cocaine)
Tip
Serotonin syndrome rarely occurs with a single serotonergic drug used at therapeutic doses. More commonly, it is due to the combined effects of several serotonergic medications, overdose, and/or a drug-drug interaction. E.g. a depressed patient also takes linezolid.
Pathophysiology
Clinical features
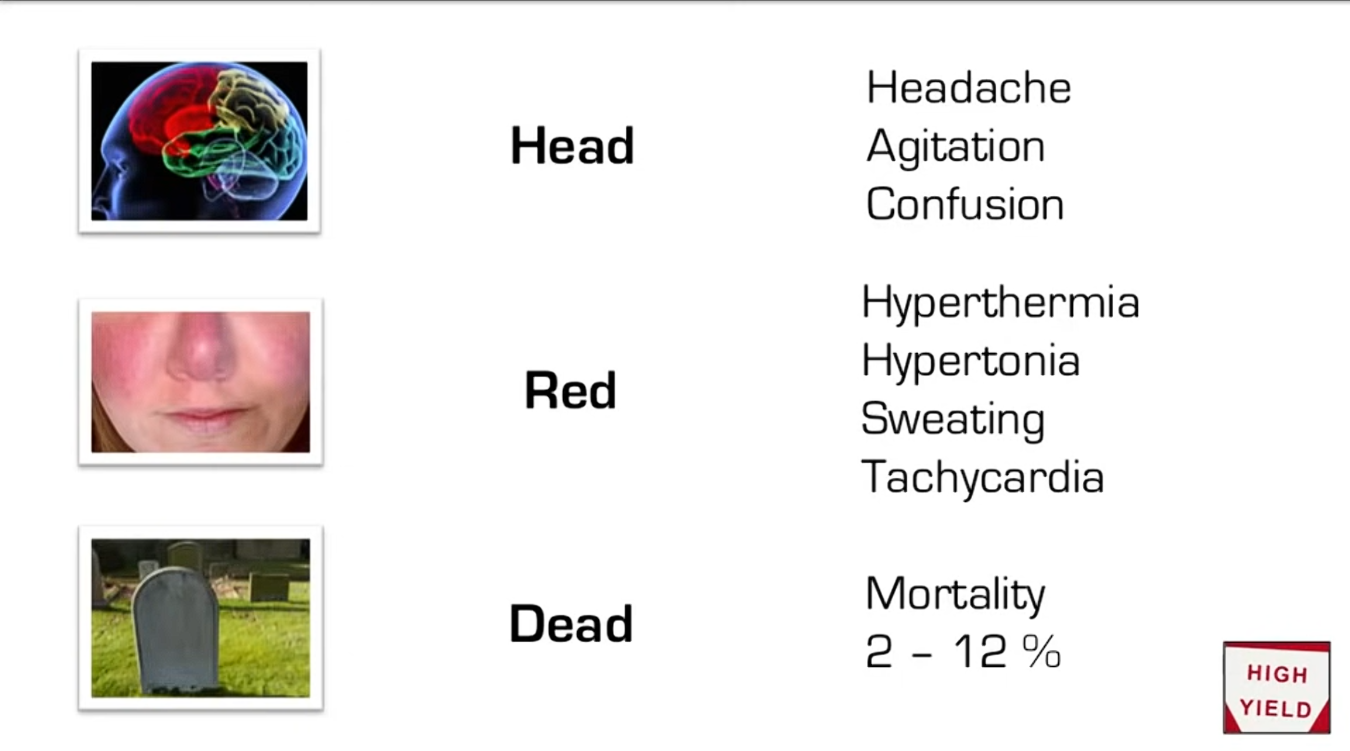
- Onset: acute, typically within 24 hours of administration of the causative drug
- Classic triad
- Autonomic dysfunction
- Diaphoresis
- Tachycardia
- Hypertension
- Mydriasis
- Neuromuscular excitability: can lead to hyperthermia
- Contrast to Parkinson disease
- Hyperreflexia
- Myoclonus
- Clonus
- Horizontal ocular clonus
- Hypertonicity
- Rigidity (especially in the lower extremities)
- Altered mental status
- Delirium
- Psychomotor agitation
- Autonomic dysfunction
Diagnostics
Treatment
- Agitation and excessive muscle activity: Treat with benzodiazepines.
- Hyperthermia: Initiate cooling measures, e.g., by reducing ambient temperature, applying cooling blankets or ice packs, administering cold IV fluids.
- Autonomic instability
- Give antihypertensive treatment.
- Treat MAOI-induced hypotension or shock.
- Moderate to severe and/or refractory cases
- Consider treatment with 5-HT2A receptor antagonists: cyproheptadine