Epidemiology
Etiology
Amyloid precursor protein (APP) gene
- Linked to 10–15% of early-onset familial AD cases
- Since the APP gene is located on chromosome 21, individuals with trisomy 21 have an increased risk of early-onset AD due to APP overexpression
- Age at disease onset usually resembles parental age at disease onset (median ∼ 49 years).
Presenilin-1
- Earlier onset compared to AD due to mutations of other genes (median is ∼ 43 years)
Apo ε
- Apolipoprotein E (ApoE)
- Risk of late-onset AD increases with the number of carried Apo ε4 alleles.
- Apo ε2 alleles may have a protective effect (reduce the risk of late-onset sporadic AD).
Pathophysiology
Mnemonic
PArkinson’s Disease = doPAmine Dowm Alzheimer Disease = Acetylcholine Down
- Senile plaques (neuritic plaques)
- Extracellular
- Located in the grey matter of the brain
- Aβ protein is the main component of the plaques.
- Enzymatic cleavage of transmembranous APP by β-secretase and γ-secretase → Amyloid beta (Aβ) peptide aggregation → formation of insoluble plaques → neurotoxic effect
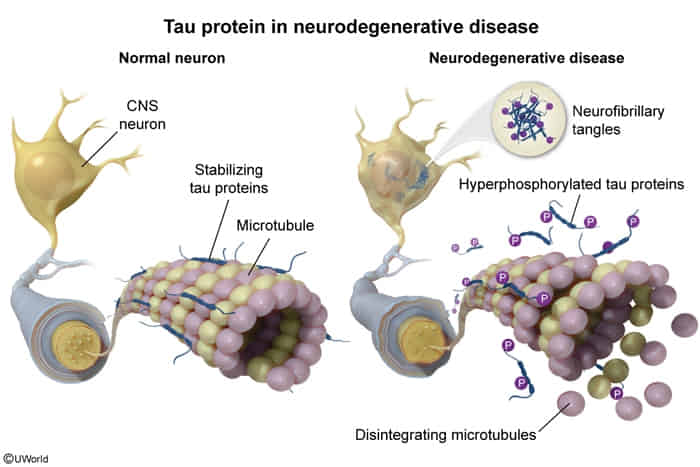
- Neurofibrillary tangles
- Intracellular
- Tangles are composed of hyperphosphorylated tau protein (an insoluble microtubule-associated protein).
- Tau is a protein associated with neuronal microtubules. Under normal conditions, tau takes part in microtubule stabilization. In AD, tau is hyperphosphorylated and disassociates from the microtubules, which may lead to instability and disrupted axonal transport. Hyperphosphorylated tau also makes paired helical filaments, which create intracellular neurofibrillary tangles, resulting in neuronal damage. Increased accumulation of these tangles is associated with progression of AD.
- Reduced cholinergic function
- Acetylcholine deficiency is related to the degeneration of cholinergic neurons and likely plays a role in the decline of cognitive abilities.
- This occurs due to a deficiency of choline acetyltransferase.
- The decline in acetylcholine is most notable in the nucleus basalis of Meynert, which participates in memory and cognition. This nucleus is located at the base of the forebrain and widely projects to the neocortex.
- Another involved structure is the hippocampus: The major function of the hippocampus is the formation of new memories.
Clinical features
Cognitive
- Common symptoms of cognitive impairment
- Short-term memory impairment
- Insidious onset
- Slow progression
- Episodic memory affected first
- Language impairment
- Typical sequence: impaired naming, followed by impaired comprehension and impaired fluency
- Temporal and spatial disorientation (patients are usually not oriented to person, place, time, or events)
- Impairment of executive functions and judgment
- Short-term memory impairment
- Less common symptoms
- Primary progressive aphasia
- Apraxia
Noncognitive
- Behavioral changes
- Apathy
- Agitation, aggression, irritability
- Mood disorders (e.g., symptoms of depression)
- Urinary incontinence
Diagnostics
MRI brain
- Indication: all patients as part of the initial evaluation of major neurocognitive disorder
- Supportive findings
- Signs of generalized or focal cerebral atrophy
- Enlarged ventricles (ventriculomegaly)
- Narrowing of gyri
- Prominent cerebral sulci (hydrocephalus ex vacuo)
- Disproportionate atrophy of the medial temporal lobe including the hippocampi, amygdala, cingulate cortex, and parahippocampal gyrus
- Signs of generalized or focal cerebral atrophy
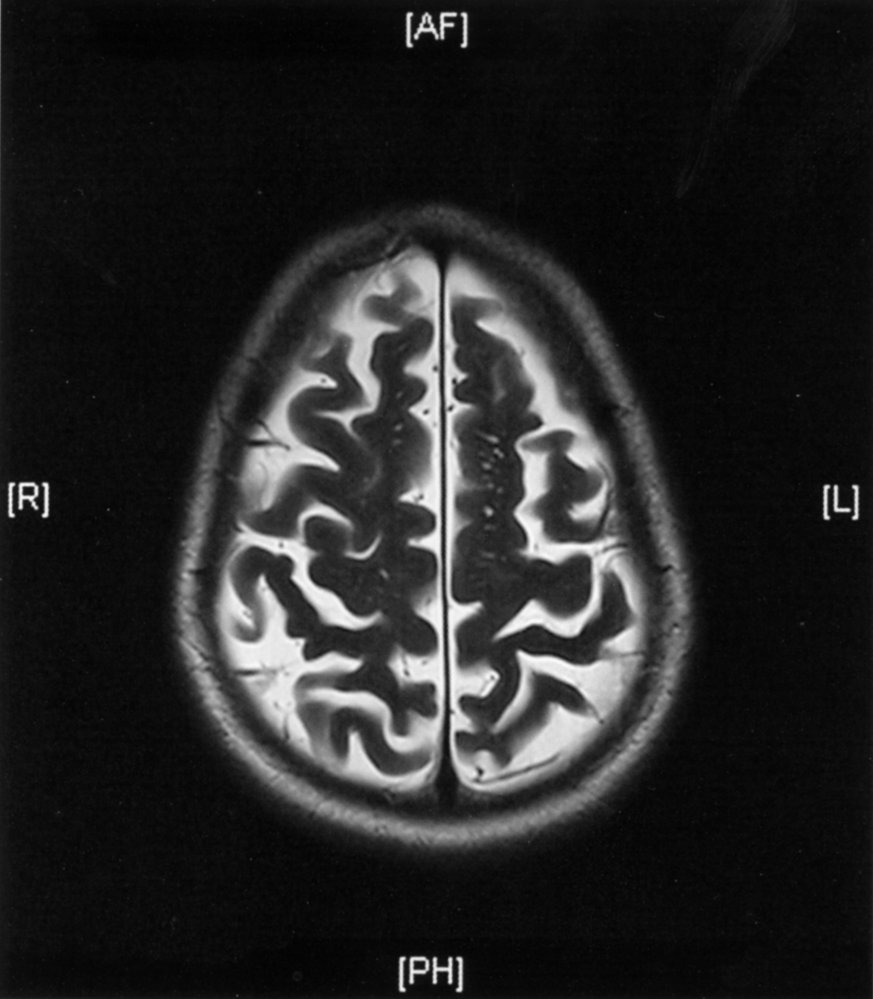
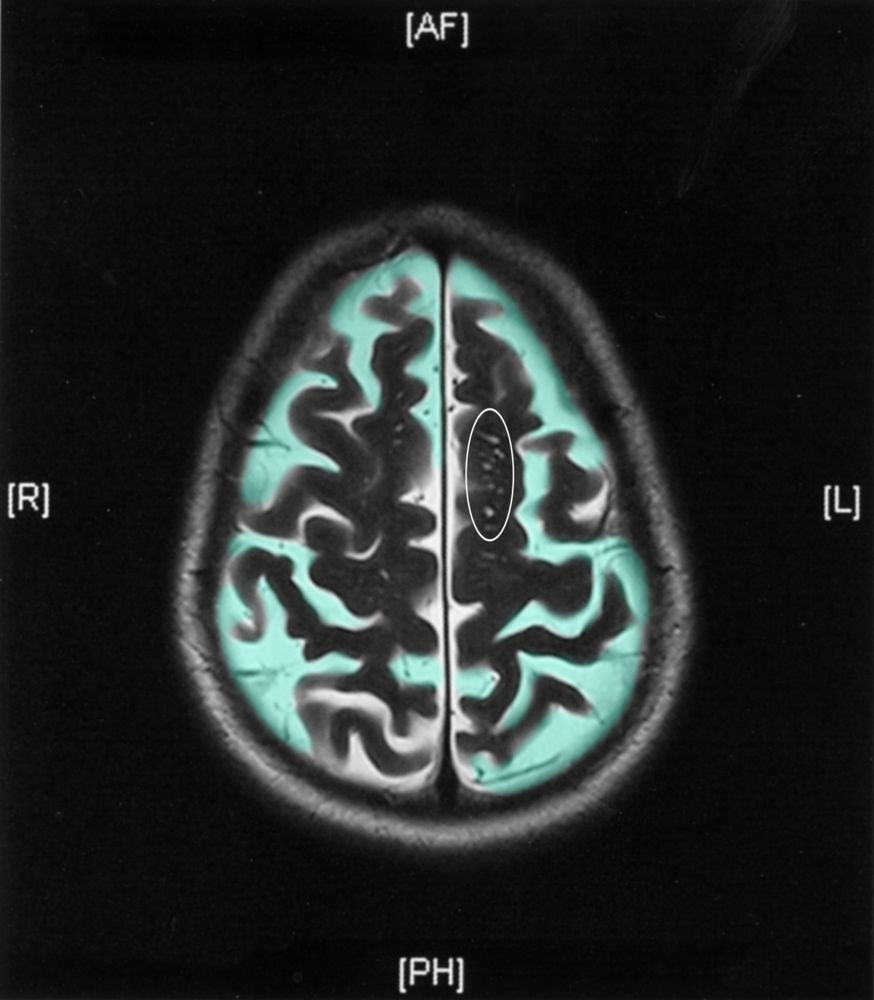 There is bilateral cerebral atrophy, with prominent sulci (green overlay). Multiple small hyperintense foci in the white matter (examples outlined) are enlarged perivascular spaces (Virchow-Robin spaces).
There is bilateral cerebral atrophy, with prominent sulci (green overlay). Multiple small hyperintense foci in the white matter (examples outlined) are enlarged perivascular spaces (Virchow-Robin spaces).
Pathology
Macroscopic
- Cerebral atrophy
- Damage to the hippocampus and parahippocampal cortex (medial temporal lobe structures) is the earliest gross pathological change.
- Degeneration of cholinergic neurons in the nucleus basalis of Meynert
- Diffuse cortical atrophy occurs as the disease progresses.
Microscopic
- Amyloid beta (Aβ): stains with Congo red under polarization
- Cerebral amyloid angiopathy
- Multiple large red-brown extracellular senile plaques (beta-amyloid core) in gray matter
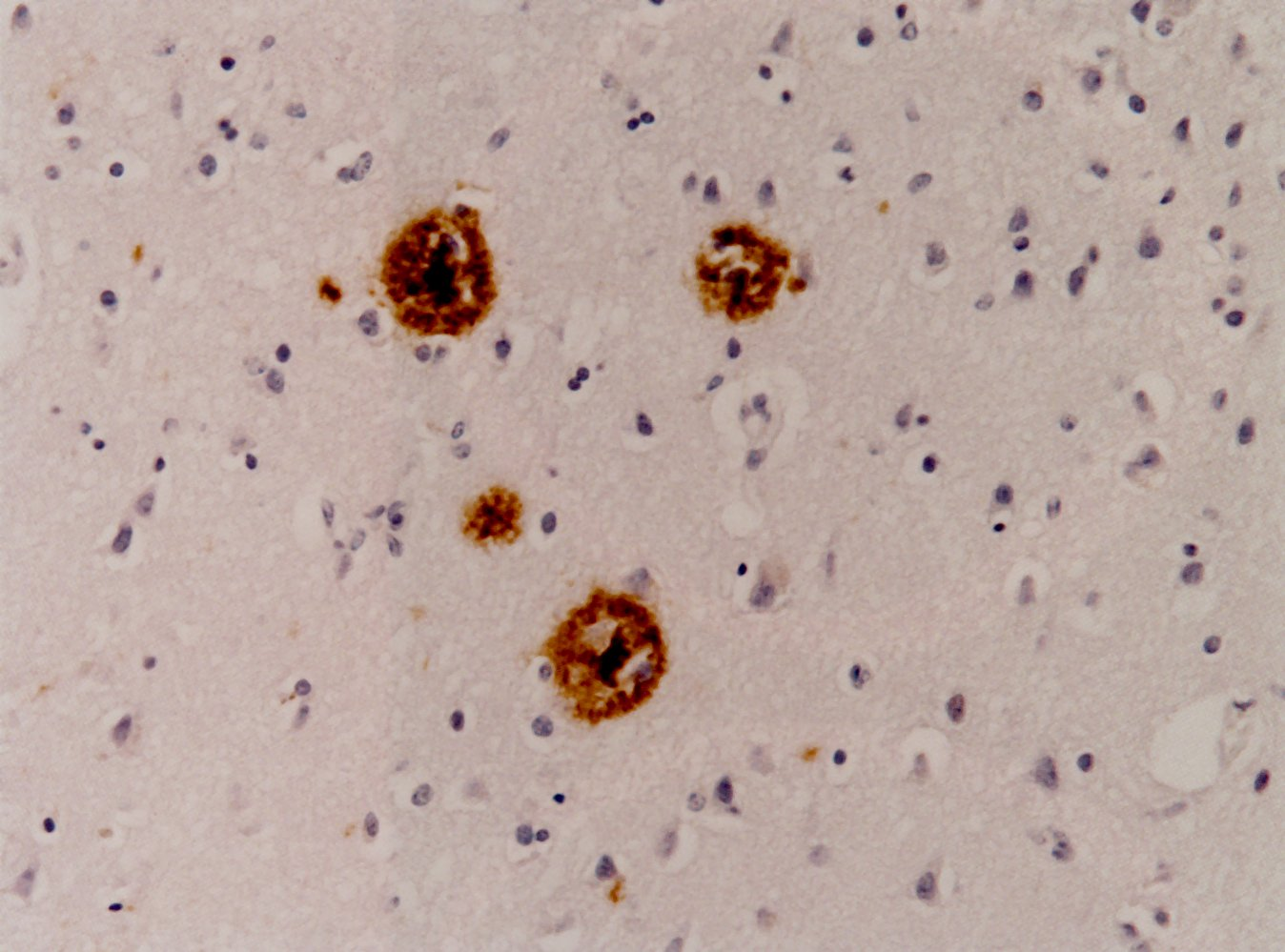
- Tau protein: intracellular neurofibrillary tangles that stain with Gallyas silver
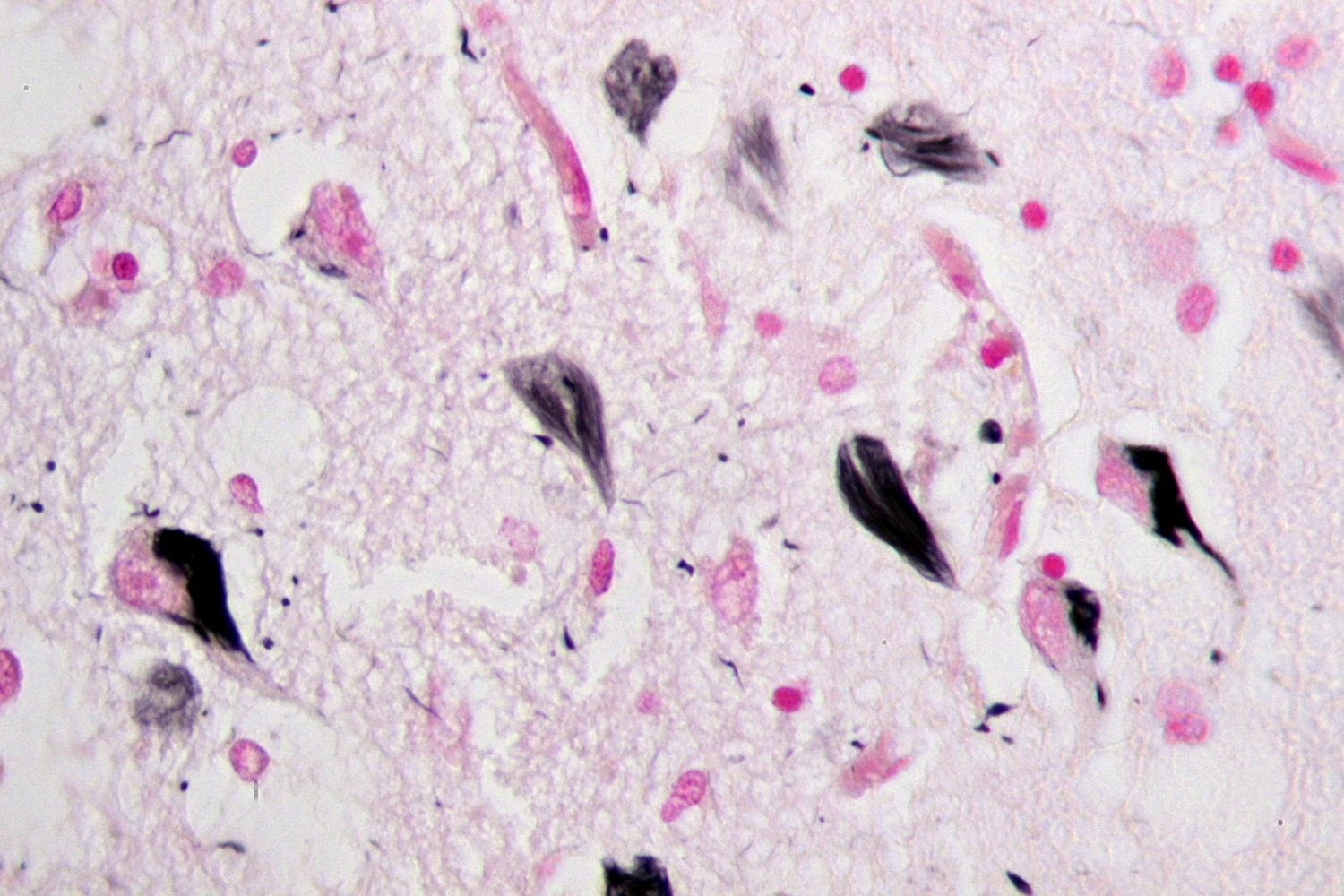
- Hirano bodies
- Intracellular rod-shaped eosinophilic aggregates of actin and actin-associated proteins in neurons, especially in hippocampus
Treatment
Pharmacological treatment
- Acetylcholinesterase inhibitors (AChEIs)
- Rivastigmine, Galantamine, Donepezil
- Mild to moderate AD (first-line)
- Reversible cholinesterase inhibition → ↑ ACh concentration at the synaptic gap
- Adverse effects
- Nausea, vomiting
- Dizziness
- Insomnia
- Cholinergic crisis
- Bradycardia, conduction abnormalities
- NMDA receptor antagonist: memantine
- Moderate to severe AD; Often used in combination with donepezil
- NMDA receptor antagonism → ↓ glutamate-induced calcium-mediated excitotoxicity
Tip
Pharmacological therapies provide only modest delay in the progression of cognitive decline, with no change in disease course.