See also Lipid transport
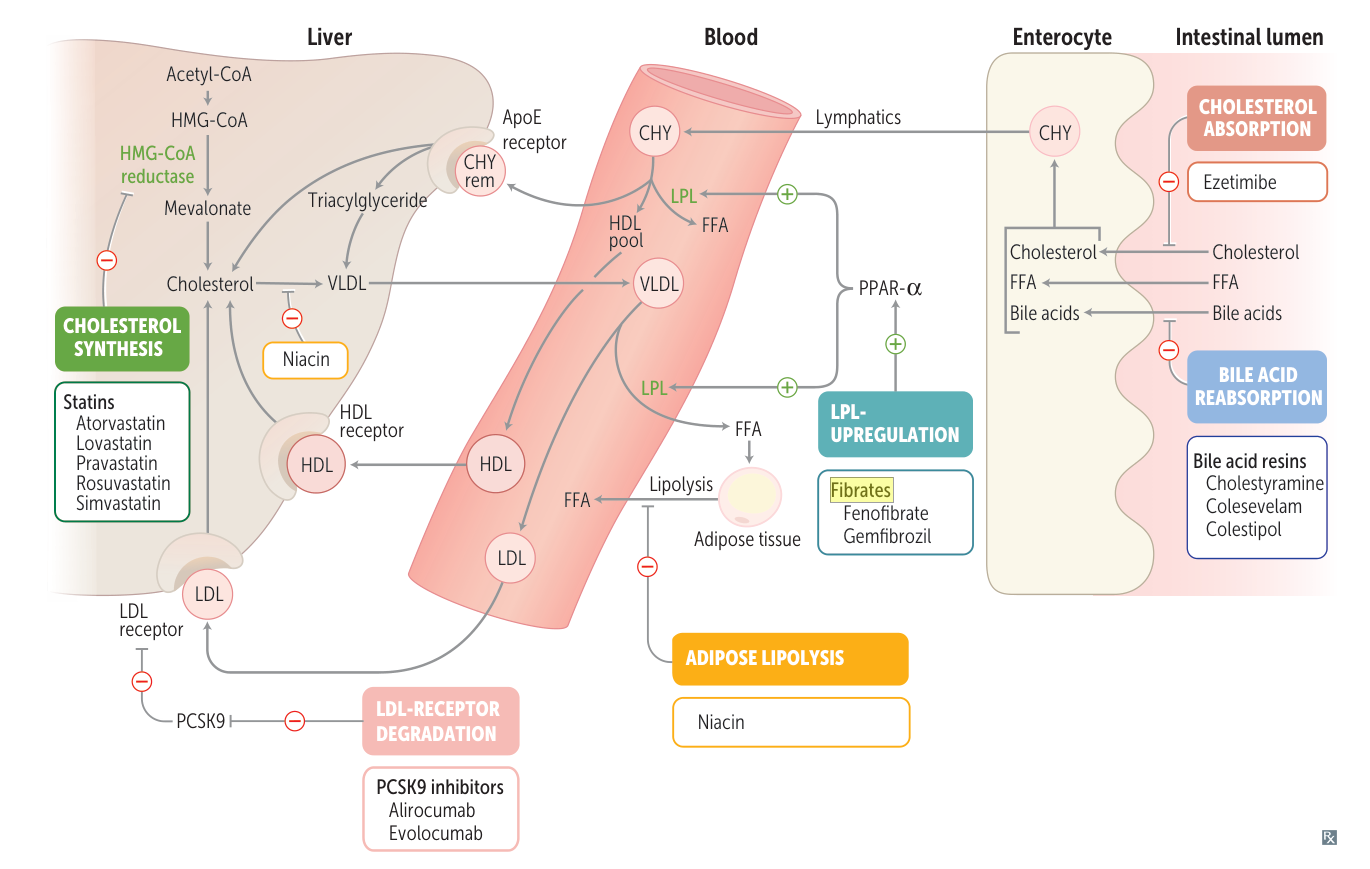
| Lipid-lowering therapy | LDL cholesterol | HDL cholesterol | Serum triglycerides |
|---|---|---|---|
| Statins (atorvastatin, rosuvastatin, simvastatin) | ↓↓ | ↑ | ↓ |
| Fibrates (fenofibrate, gemfibrozil) | ↓ | ↑ | ↓↓ |
| Bile acid sequestrants (cholestyramine, colesevelam, colestipol) | ↓ | - | ↑ |
| Niacin | ↓ | ↑↑ | ↓ |
| Ezetimibe | ↓ | - | ↓ |
| Omega-3 fatty acids | - | ↑ | ↓ |
| Exercise & weight loss | ↓ | ↑ | ↓↓ |
Statins
- The only first-line medication for dyslipidemia, significantly reducing the risk of mortality in patients suffering from CAD.
- Competitive inhibition of HMG-CoA reductase renders this enzyme unable to convert HMG-CoA to mevalonate (the rate-limiting step of cholesterol synthesis) → reduced intrahepatic cholesterol biosynthesis → upregulation of expression of LDL receptor gene via sterol regulatory element-binding protein (SREBP) → increased LDL recycling and:
- ↓↓ LDL cholesterol
- ↑ HDL cholesterol
- ↓ Triglyceride level
- Adverse effects
- Statin-associated myopathy
- Muscle pain and weakness, especially when used alongside fibrates or niacin
- Myositis: ↑ CK
- Statins are metabolized by CYP3A4. This enzyme can be inhibited by macrolide antibiotics (eg, erythromycin, clarithromycin), leading to increased statin drug levels and subsequent statin myopathy. See Cytochrome P450.
- May progress to rhabdomyolysis: rare but severe side-effect that may lead to myoglobinuria → AKI (↑ BUN and ↑ creatinine)
- Treatment must be discontinued if myopathy/rhabdomyolysis occurs.
- Statin-associated myopathy
Ezetimibe
- Mechanism of action: selective inhibition of cholesterol reabsorption at the brush border of enterocytes (cholesterol transporter NPC1L1) → ↓↓ LDL, little effect on HDL (slight ↑) and triglycerides (slight ↓)
- Adverse effects: ↑ Liver enzymes
Mnemonic
EzetimIBe — Intestinal brush border
Fibrates
- Agents: bezafibrate, fenofibrate, and gemfibrozil
- Mechanism of action: activation of the peroxisome proliferator-activated receptor alpha (PPAR–α) → ↑ lipoprotein lipase activity → more rapid degradation of TGs circulating in chylomicrons and VLDLs into fatty acids and glycerine, which can be taken up by cells; and induction of HDL synthesis → ↓ LDL, ↑ HDL, ↓↓↓ triglyceride
- Adverse effects
- Dyspepsia
- Myopathy, especially in combination with statins
- Cholelithiasis: fibrates inhibit cholesterol 7α hydroxylase → decreased bile acid synthesis → supersaturation of bile with cholesterol (↑ cholesterol:bile acid ratio)
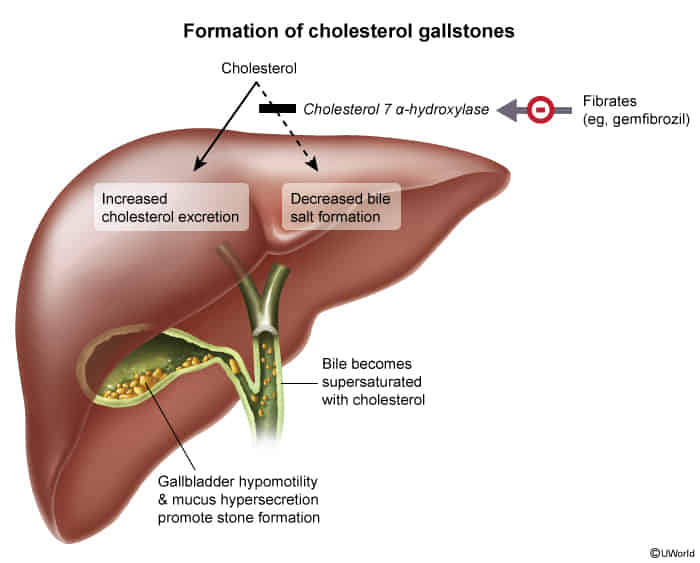
- ↑ LFTs (reversible)
Tip
Pioglitazone activates PPAR-γ. See Diabetes mellitus > T2DM
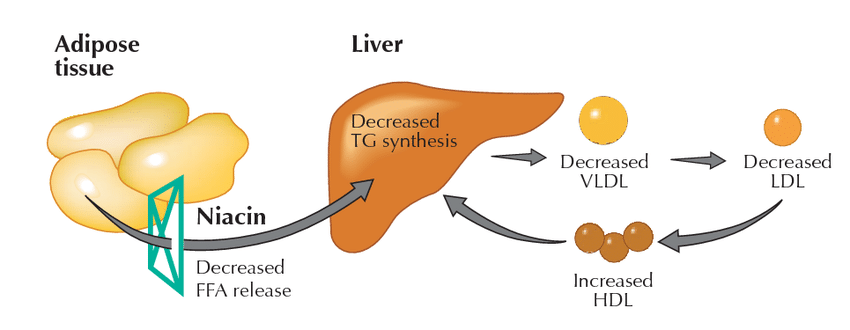
Niacin (Vitamin B3)
- Mechanism of action: inhibits lipolysis and fatty acid release in adipose tissue through blockade of hormone-sensitive lipase and ↓ hepatic VLDL synthesis → ↓ triglyceride, ↓↓ LDL synthesis, ↑↑ HDL
- Indication: high LDL cholesterol and lipoprotein(a) levels (> 50 mg/dL) despite statin and ezetimibe therapy (or if statins are contraindicated)
- Adverse effects, see Vitamin B3 > Vitamin B3 toxicity
- Flushing and pruritus
- Hyperglycemia
- Hyperuricemia and gout
- Niacin decreases renal uric acid excretion.
Bile acid resins
- Drugs: cholestyramine, colestipol, colesevelam
- Mechanism of action
- Ion exchange resin binds bile acids in the intestine → interruption of enterohepatic circulation (↓ bile acid absorption and ↑ bile acid excretion) → ↑ conversion (compensatory) of cholesterol to bile → lowers cholesterol pool in the liver and promotes synthesis of LDL receptors and ↑ LDL receptor recycling → ↓↓ unbound LDL, slightly ↑ HDL, and slightly ↑ triglycerides
- Indications
- Combination treatment with statins in hypercholesterolemia
- Digitoxin overdose
- Adverse effects
- Gastrointestinal: nausea, abdominal bloating and cramping